Cooking Burn Care Expert Advice
Learn how a doctor treats her own second-degree kitchen burn, including tips on pain management, dressing changes, and infection prevention.
On July 9, I was outside grilling some extra fatty beef (73% lean/27% fat) burgers on a natural gas grill with ceramic briquettes. The high fat content makes them so good. They don't dry out even when I make the burgers well done. Unfortunately, the high fat content may have contributed to the whole issue. I use aluminum foil on the grill for easier clean up so the burgers get nice grill marks without making a mess dripping on the white briquettes, and the beef sizzle on top of its own fat, making it basically non-stick. It's really a good system, I thought. I still think it is, but I should have worn long heat-resistant grill gloves.

I should have been wearing these grilling gloves to prevent the whole mess. Lesson learned.
As I was flipping the burgers with tongs, some of the beef juices dripped off, got super heated, turned to steam, and forced up a giant splatter of oil onto my bare forearm. It was in slow motion in my head, like how some people describe near-death experiences. Obviously, it wasn't that bad, but I do remember more detail than I should. I heard the giant sizzle, heard a loud splat, felt the splat on my arm, and thought to myself, "That's going to burn - water." I briefly considered dunking my arm in the pool, but our 90-degree days meant that the pool water was at bath-water temperatures. I dropped my tongs on the ground and ran inside, scaring our cat guarding the door. I ran my arm under the cool kitchen sink water for about a minute. I washed off the oils with soap and made sure that the area had cooled down. It was mildly red and a moderately painful within the first minute. There was no immediate blister, and even the redness wasn't that pronounced. I didn't run it under cool water for 10-20 minutes as normally suggested. But because it was annoyingly painful (4 out of 10 on the pain scale), I figured it would be at least a first degree burn, and I should treat it accordingly.
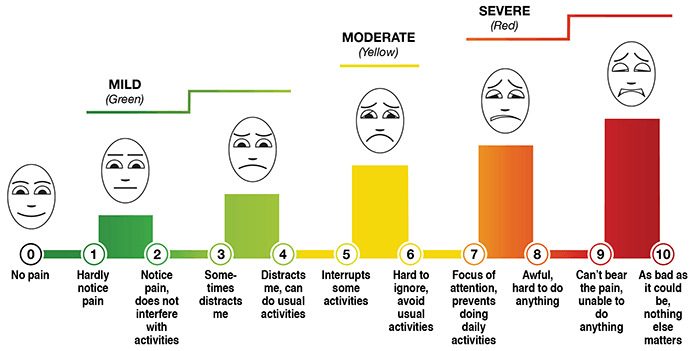
This is the standardized pain scale you may find at healthcare facilities in the US.
I'm terrible at following my own instructions as a doctor. After the initial cooling down and washing off, I put on oven mitts and flipped the rest of the burgers along with the veggies I was grilling. That took probably 3-4 minutes. Then I went back inside to properly tend to the wound because it was really starting to hurt. Ideally, I would have spent those 3-4 minutes still running my arm under cool water.
How do you tell if a burn is 1st, 2nd, or 3rd degree? Here are the burn category basics. A first degree burn has skin surface redness and is mild-moderately painful. A second degree burn has blisters and is moderately painful. A third degree burn can be extremely painful at the edges and involves tissues beyond the surface skin. It actually gets down to the fatty layer, past the nerves on the surface skin. With damaged nerves, the center of the third degree burn is may not be painful. A fourth degree burn goes all of the way down to muscle or bone. Any burns beyond a second degree burn should not be treated at home. Also, any burns with an area larger than the dressing pads sold at your local pharmacy (approximately a 3 inches by 3 inches) should be seen by a healthcare professional.
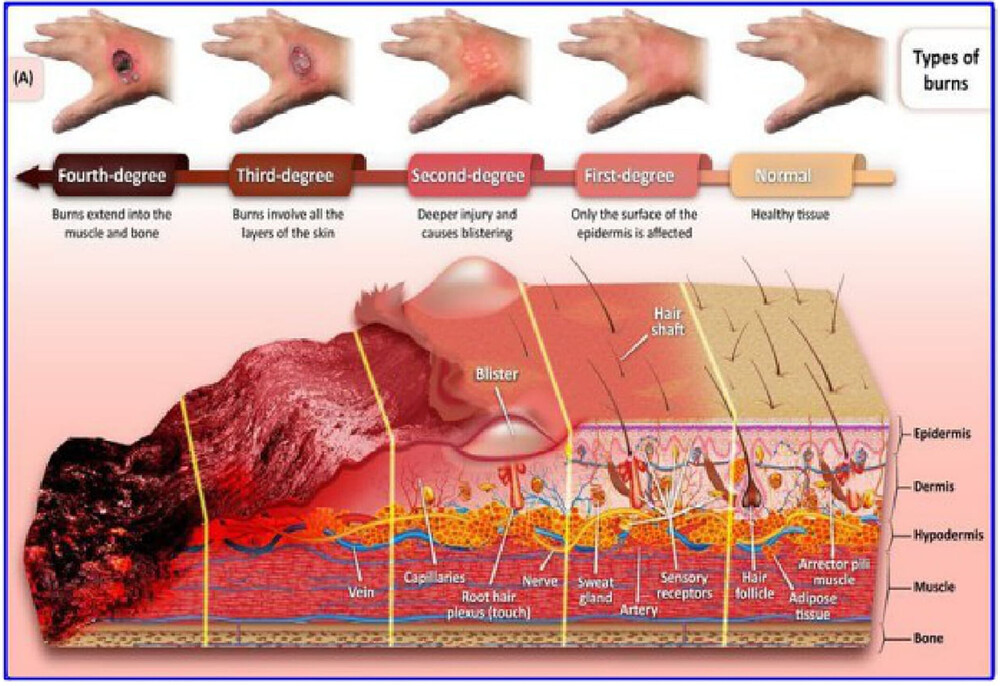
This cross-section of varying degrees of burns is from Trends in Biotechnology Volume 36, Issue 9, P907-922, September 2018.
I dug up some hydrogel that I recently bought when Rite-Aid went out of business and everything was on clearance. Hydrogel is the medical term for what might be labelled as a "moist burn pad." It's made of similar absorbent material as what's used in diapers, but in a nice, clean flat sheet pre-loaded with sterile water. (Don't use diapers obviously. It's just cool science that water-absorbing gel is in so many disparate things like the now-banned water beads toy, moisture controlling potting soil, fake snow, gel ice packs, etc.) It doesn't stick to the wound as long as it doesn't dry out. Because it's mostly water, it feels cool, and it sticks to the skin like jello. It's professional-grade stuff that's used in wound care clinics and burn centers for first and second degree burns, and all major pharmacies have it now.

The hydrogel itself is in between a sheet of blue and a sheet of clear plastic. Peel off the blue plastic and stick that side to the wound. The clear plastic helps seal in the moisture and allows you to monitor the wound without removing the hydrogel pad.
Within 10 minutes, I had fully rinsed, washed, cooled, and applied the most appropriate dressing for the burn. Over the hydrogel pad, I wrapped a few layers of gauze to keep it on. Over the gauze, I wrapped an ice pack. Over that, I wrapped more gauze to keep the ice pack on. Don't put an ice pack directly on skin. If it's cold enough, it can freeze the skin, which just makes things that much worse. You don't need a frost bite along with a burn. I was using the ice pack to keep the burn cool and to keep it from hurting so much. It was over the hydrogel and several layers of gauze. In those first few hours, the pain was significant. Without rotating out the ice packs every 20 minutes, I would have been crying.
I made a quick trip to the store to see what was available and came home with Alocane Max. It's a liquid gel with 4% lidocaine, a topical anesthetic. Topical means on the skin. Anesthetic is a numbing agent. Lidocaine applied to the burn numbs the area and stops it from hurting. It's the same stuff that I used to inject into the skin before stitching it up or cutting out a cyst. It's very effective at numbing for a few hours. Lidocaine can also be used to make the heart beat differently. Lidocaine at the right time helps fix irregular heart rhythms, and at the wrong time causes irregular heart rhythms. You don't want this stuff going to the heart at the wrong time. How might it go to the heart at the wrong time? Through excessive absorption when there's a large, open, bloody wound exposing blood vessels that could carry the lidocaine quickly to the heart. It's extremely unlikely to absorb enough to cause heart problems when used correctly, but heart issues is why you need to follow the instructions on the packaging. If a wound is bleeding or was recently bleeding, don't apply anything with lidocaine. The box says you can use it up to 3 times a day.
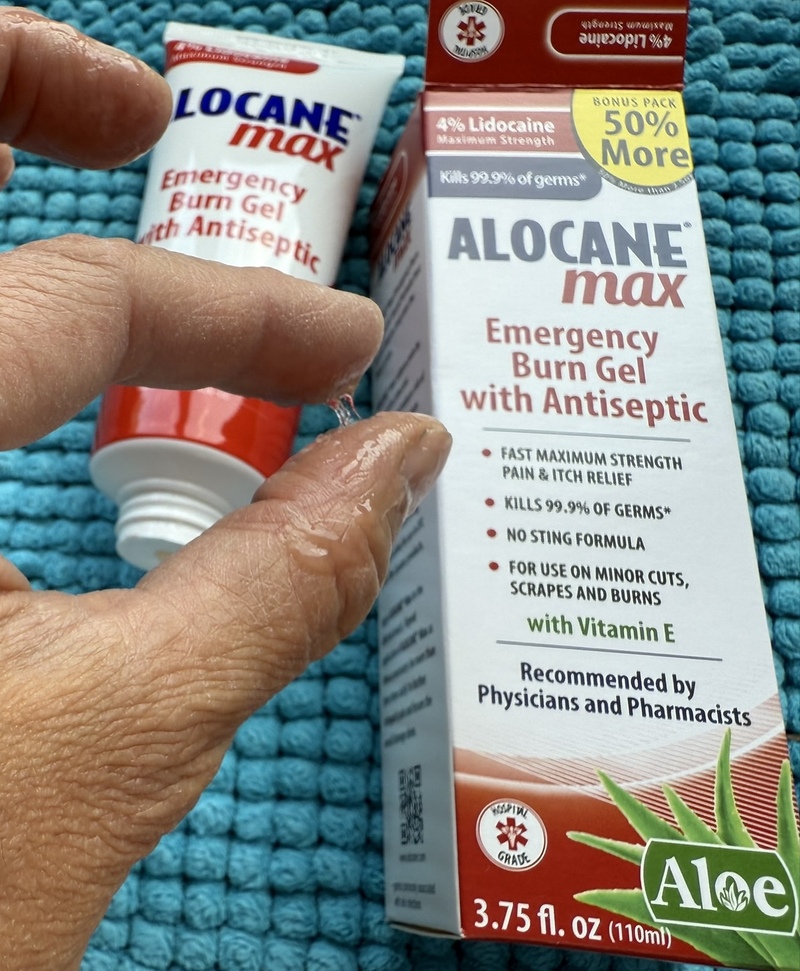
Alocane gel is mostly Aloe, so it's a sticky goop. It also contains lidocaine as an anesthetic and benzalkonium chloride as an antiseptic.
About 2 hours after the burn, I re-dressed the burn with Alocane. At bedtime, I redid the whole thing again with fresh Alocane, new hydrogel pads, and layers of gauze. The lidocane helped so much by bedtime that I didn't need to use any more ice packs. I normally have some carpal tunnel symptoms, so I always sleep with a wrist brace. I just loosened my wrist brace and use that as another dressing stabilizer.

The carpal tunnel wrist brace helped to hold the burn dressing in place.
The burn appeared to be just a first degree burn that first evening. I didn't take any pictures of it because I didn't find it remarkable in any way other than the pain. The area was pink and unimpressive. The next morning, I applied fresh Alocane Max to prevent the area from hurting and to keep it moist since the gel was starting to dry. It actually didn't hurt much by the next day. With it wrapped, I was able to have a fairly normal day, using my arm for all sorts of normal activities other than direct pressure on the burn. In the early evening, I was heading out for an event so I re-dressed it. That was when I first noticed some sloughing skin that would eventually grow into a blister.

There is a small portion in the middle of the burn where the skin is lifting off, suggesting a second degree burn surrounded by a first degree burn.
I placed a fresh hydrogel pad on it, wrapped, and decorated the area with an excessive number of bracelets so it wasn't obviously a wound. I didn't want to have to explain the whole thing all evening as it was a kid-centric event. No one noticed (except another doctor), so the ruse worked!

These bracelets covered and protected the burn, holding the hydrogel in place.
By bedtime (about the 30 hour mark), the blisters had popped up. I bought a hydrogel pad designed for new moms because that was the only hydrogel at Target. Walmart was sold out, and all of the pharmacies were closed by the time the event finished. As it turns out, it was the perfect size and worked really well. The second night, all I needed was the hydrogel pad, gauze to hold it in place, and my carpal tunnel brace.

These Frida mom hydrogel pads are the most cost effective hydrogel pads, and they last 8-12 hours for burns. The drawback is that you can't see through it because one side is a thin felt-like surface. If you intend to change the hydrogel a few times a day, and the wound doesn't require close observation, these can cost less than $1 each as opposed to $3 each.
The next day, with multiple blisters popping up but still staying intact, I continued to use the hydrogel pad and gauze. When blisters aren't popped, there's little risk of infection. The wound isn't open to germs, so antimicrobials like antibiotic cream aren't necessary. As soon as a burn blister pops though, the risk of infection is much higher. The larger the area and the dirtier the area, the riskier. My forearm is very low-risk.
- The area is easy to keep clean.
- It's easy to wash, dry, and keep dry.
- I can see the whole thing very well.
- Circulation there is good.
- I don't have to put direct pressure on it for any reason.
- I don't have diabetes and am not immunocompromised.
- The combined total area of burn is less than 10 square centimeters, and the second degree portion is only 3 square centimeters.
By bedtime that third night (over 50 hours since the burn), the area was starting to itch. Itching is good and bad. Itching means that it's starting to heal. The worst is over, and the body is starting to fix the problem. It should not get worse as long as it doesn't get infected. The bad thing about itching at bedtime is that it's impossible to prevent scratching, even with lots of layers of dressing. The same nerve cells that transmit the sense of itching are the same ones that transmit pain. From a nervous system standpoint, itching is just low-level pain. Lidocaine numbs those nerve cells, so I used the Alocane Max again that night to minimize itching. My dressing had the same layers as the first night: Alocane Max, Hydrogel pad, gauze wrap, and wrist brace.
Unfortunately, I managed to scratch under the gauze and pop all of the blisters by the next morning. I have a vague dream-like memory of pain when one of the blisters popped. When you peel back the hydrogel, you can see the raised areas, some with yellow. The raised areas are where the hydrogel absorbed extra fluid that the wound leaked. You can also see some slightly yellow bits. That exudate (leaked body fluids) is made up of blister fluid and some white blood cells that are repairing and cleaning up the mess. It's a normal part of the healing process as long as it's not getting increasingly yellow over time, turning green, smelling bad, getting cloudy, feeling more painful, looking like cloudy gray pus, or changing from non-bloody to bloody. Those are all signs of infection, which usually show up 24-72 hours after blisters pop.

When you peel back the hydrogel, you can see three patches of yellow exudate where the skin wound was leaking fluid.
Once a blister pops, bacteria start to enter. Your body may be able to naturally keep things under control, but burns tend to be large wounds, so infections are common. New wound priorities:
- Create an antimicrobial environment to prevent infection.
- Keep the area moist for the prettiest healing (dry scabbing wounds scar worse than wounds allowed to heal while moist).
- Relieve continued itching (an annoyance issue during the day but also a real infection risk at night with inadvertent scratching).
To minimize risk of infections, there are a few things to use. If the blistered area is large enough and there is enough fluid leaking out that soak the hydrogel, expanding it, you'll want it to get a little dryer. Silver alginate looks like a gray felt pad and is excellent for absorbing fluid, getting soft to conform to the wound, and using silver to kill off microbes. Silver acts as an antibiotic and keeps all sorts of microbes at bay. You'll want to use the silver alginate only if there is enough fluid leakage to wet the silver alginate pad AND keep the wound moist. When silver alginate gets wet, it turns into a gel and smell a little funny. Alginate is actually made from seaweed, so silver alginate smells like metal and plants. You can cut off a little portion of it and put it in water to get a sense of the "normal" smell. If a wound smells "bad" and different from that normal smell, that's concerning. You can cut the silver alginate to cover the wettest portions of the wound. Then cover the entire thing with either a slightly larger hydrocolloidal bandage (not hydrogel), a transparent waterproof film like Tegaderm if you need to keep it water resistant (such as a burn on the hands), or just plain gauze for areas less likely to get wet. I tried it briefly, but it was clear that the blisters weren't exuding enough fluid to wet the silver alginate and stay moist.

Use silver alginate pads directly on a wound that is leaking a lot of fluid to control the moisture level while providing an antimicrobial environment.
If there is not enough fluid leakage to keep the wound moist, then use a gel with silver nanotechnology: Silvex wound gel. We used to use a white thick ointment called silver silvadene, but that's an outdated cream now. Nano silver is better, and there's no sulfa to cause sulfa allergic reations. The nano silver neutralizes microbes, and the gel keeps the wound moist. This is what I ended up using because my wound is relatively small and not leaking much.
Silvex is a better choice than Alocane Max once the blister pops. Alocane Max has Lidocaine, so should not be applied more than 3 times a day. The antiseptic in it is benzalkonium chloride, which is usually used for cleaning surfaces. A lot of sanitizing hand wipes use it to clean germs off hands, in the same way we used to use ammonia to clean bathroom floors. It's designed for skin surfaces, not for penetration or lingering. The nano silver in Silvex kills bacteria too, penetrates better, and doesn't evaporate off.

Silvex wound gel contains silver to combat a wide range of infection-causing microbes. Apply a generous layer to the burn.
There is no need to remove the old skin that was covering the blister. It's a nice protective layer unless the area gets infected. If there is an infection, of course you'll need to visit a health clinic and any material (old dead skin) that bacteria could grow on should be removed if possible. Burn care is a serious art and science mixed with a lot of pain, smells, and a long list of wound coverings. If a burn is beyond home management, take it seriously and get professional help.
I am currently in the fourth day after the burn. The area is doing what it's supposed to be doing: leaking out a bit of clearish fluid (absorbed on the hydrogel), itching a lot, not turning red, not painful, not changing too much. I plan to continue this dressing plan for the next few days:
- silvex gel
- hydrogel pad
- gauze wrap
I'll change it at bedtime, upon waking, and in the afternoon if I'm particularly active that day or if it could be dirty. I would expect continued healing with new skin starting to form under the blistered part over the next few days. The old dead skin previously covering the blister will probably fall off around the 1 week mark. As long as there is a thin layer of new skin showing up, I won't need to keep the area consistently moist anymore. The dressing can be simplified to just a gauze wrap for protection.

For a burn wound, apply a medicated gel, cover with hydrogel, and secure with gauze or tape. Download these instructions in PDF format.
A few things to note:
- A hydrocolloidal patch is not the same thing as hydrogel. Hydrocolloidal patches are designed to absorb moisture. They are also sticky, so they can easily take off the top layer of a blister. Hydrogel have no adhesive. They are like jello and won't disturb a blister. They help maintain the perfect moisture balance for the skin, absorbing excess moisture and replenishing moisture when necessary.
- The most cost-effective hydrogel patches I found was actually the Frida Mom Cooling Hydrogel Nipple Pads. Unlike what the box says, you don't have to change it every 4 hours for first or second degree burns. Just change it when it starts to dry out, which is more like 12 hours. If it gets too moist and swells, you should be using silver alginate instead.
- The Alocane emergency burn pads are unfortunately just a cotton pad with their gel, not a hydrogel pad with lidocaine. It dries out in a few hours and must be changed before drying out. If it dries, it becomes very painful to remove and can take off the top of a blister.

Alocane emergency burn pads are just gauze with some alocane gel. I recommend buying the gel as it's more cost effective and flexible.
Updates
July 14
During last night's dressing change, the lower portion of the wound with the open skin was a bit swollen and pink. The pink swollen area extended about 2-3cm (an inch) around the wound. That's a sign of an infection. Infections are characterized by the Latin mnemonic dolor (pain), calor (heat), rubor (redness), and tumor (swelling). As it was Sunday night, I figured I'd put extra Silvex on it, wrap it extra so I don't mess up the dressing during sleep, and check it first thing in the morning.
When I checked it this morning, the redness and swelling had gone down. There was no obvious delineation between infected skin and normal skin anymore, so I couldn't put a measurement to it. I put more Silvex on it and will continue to monitor it throughout the day.
Do you see the edges of the infection? It's just starting, so it's very subtle. The area is slightly swollen, and there is a subtle area of pink around the open wound. It didn't hurt much, and I felt fine otherwise. With appropriate treatment, the infection subsided and was visibly improved 12 hours later. The area is no longer swollen, as demonstrated by the return of skin lines. There is also far less pink. I'd say probably half of the original diameter. It's heading in the right direction.
Had it stayed the same or gotten worse, I would have booked an appointment with my primary care doctor for today to get antibiotics. If something needs antibiotics, the sooner the better. If my usual doctor's office was too busy, I would have looked into urgent care or an online virtual doctor's visit. I would have made sure to get antibiotics started before the end of the day today. Treating an infection should be always be a top priority.
If it was going to get worse, it could have started to affect my forearm function by tomorrow (30 hours) with significant swelling, red streaks of infection up to my elbow, increasing pain, and started a general mild fever and malaise. By 48-72 hours, there could be a significant general fever, achiness, and fatigue. The arm infection would be super obvious and painful, and treatment would be at the level of an emergency room visit. Without antibiotics, infections can eventually turn deadly.
July 17
It's been a full week now. The past 3 days have been uneventful. The burn is healing up nicely, and the beginnings of an infection went away. The burn surface now feels a bit rough. The open wound area still drains a little bit of exudate, so I use the Silvex there. I am no longer applying Silvex to the rest of the burn. It doesn't itch as much as it did a few days ago. Since I still have some more hydrogel, I plan to use it for the next few days for extra protection and optimal healing. However, I think it would likely be okay to just apply bacitracin ointment to the open wound portion and cover with a simple bandaid.
The open wound is now a clear ulcer. That's not necessary a bad thing. It just shows that entire epidermis was burned off and the wound has to heal up from the dermis. You can see the nice clean white circular edge healing into the middle. It's a tiny 2mm ulcer, so full healing should only take a few days as long as there is no infection. The rate is approximately 1mm a day for a relatively healthy middle-aged person.
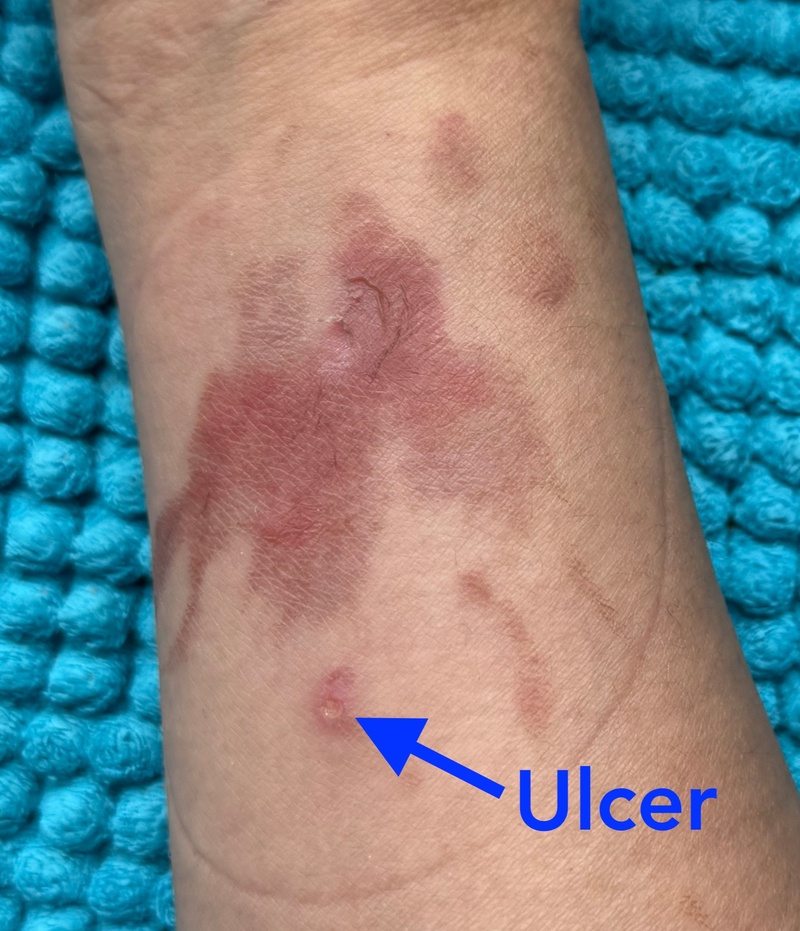
The burn is healing well. It should continue to be treated and covered due to the larger blister skin near the top coming loose and the 2mm exudative ulcer at the bottom.

cooking burn on forearm at 25 hours (day 1)

cooking burn on arm at thirty-six hours (day 2)
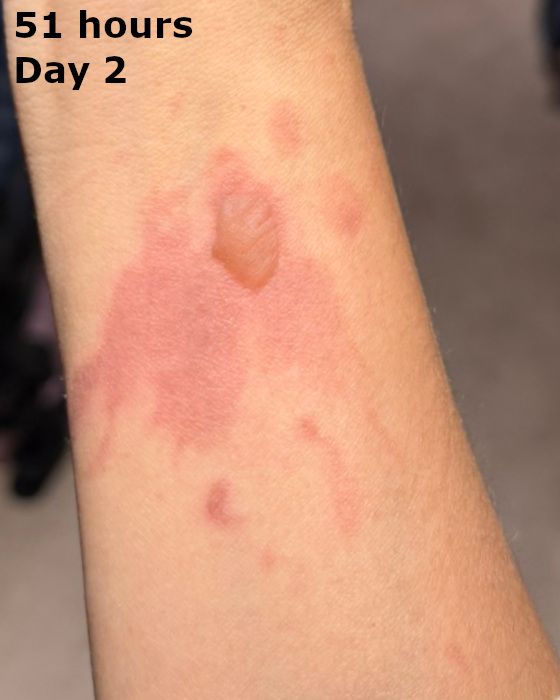
cooking burn on forearm at fifty-one hours (day 2)

cooking burn on forearm at sixty-eight hours (day 3)

cooking burn on forearm at 76 hours (day 3)

cooking burn on forearm at 88 hours (day 4)

cooking burn on forearm at 100 hours (day 4)

cooking burn on forearm at 110 hours (day 5)

cooking burn on forearm at 123 hours (day 5)

cooking burn on forearm at 137 hours (day 6)

cooking burn on forearm at 159 hours (day 7)

cooking burn on arm at 185 hours (day 8)

cooking burn on arm at 195 hours (day 8)

cooking burn on arm at 206 hours (day 9)

cooking burn on arm at day 12

cooking burn on forearm at day 15

cooking burn on forearm at day 22

cooking burn on forearm at day 29
At 2 months, the grill burn has completely healed, and the silicone scar prevention sheets have kept the scar smooth and minimal. The new skin growth is slightly more pink than the surrounding skin. Skin lines (wrinkles) have returned. Unless someone was looking specifically for the wound, it's really not obvious at all now.
The only poorly healed spot is where the infection was - the round patch at the bottom of the pictures. It's a tiny spot of magenta that's slightly indented. That spot will slowly fill in so it's less indented and the magenta will fade to a pink in about 2 years. That's in spite of using a silicone scar sheet 24 hours a day for the past 7 weeks. That's a huge difference in scarring simply because of a very mild (treated only with skin antibiotics ointment), short-lived (12 hour) infection from accidentally scratching and popping the blister while asleep. It goes to show the importance of aggressive early wound management. Just because a burn doesn't bleed like a cut, it still requires serious attention immediately. Until the skin surface recovers and the danger of infection passes (1-2 weeks for a second degree blistered burn), you should keep an eye on it at least twice daily.
I plan to use silicone sheets to minimize scarring for another month, for a total of 3 months after the injury. After that, there would be little benefit.

cooking burn on forearm at day 70
