Updates on the Coronavirus Pandemic
November 9, 2020
For the past few weeks, the news focused on the election. Hopefully you haven't missed the coronavirus stories. Cases are way up. Last week, Erie County had 149 cases, and this week, we have double - 297 cases (Nov. 2 report from Erie County). When cases go up, hospitalization goes up about a week later. Here is the current chart for Pennsylvania.

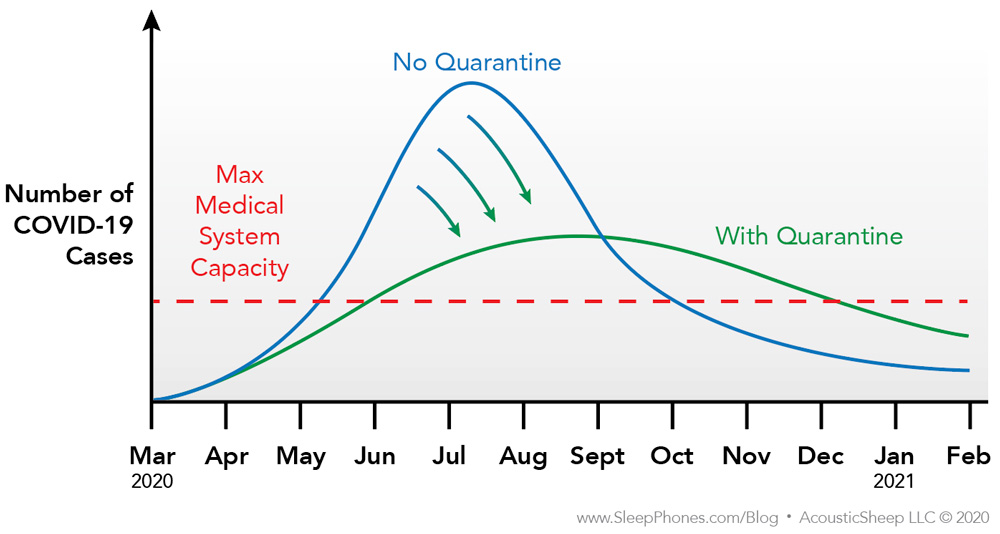
Harkening back to the beginning of the pandemic, the problem isn't simply that 0.5%-1% will die from the coronavirus, it's the overwhelming of our hospitals. You may have heard about Utah's hospitals preparing to ration care, El Paso's hospitals flying people to other cities because they've run out of ICU beds/staff, field hospitals being used in Texas and Wisconsin, and many hospital systems canceling elective procedures. If the hospitals run out of nurses who can properly administer the level of care needed, even the young people who would have lived may die. We really don't want to test the limits of our healthcare capacity with our own health.
In further bad news, we've learned about the long-term effects for people who recover. The people who survive a hospitalization often take weeks to months to recover. Many are left with months of shortness of breath, brain fog, loss of smell, and a variety of strange symptoms. Others have permanent disability from strokes, heart infections, blood clots in the lungs, and permanent reduction of kidney function. Even people with “mild” symptoms often have weeks of not being able to smell or taste anything - a symptom that scientists believe indicates an attack on some parts of the brain. While most children have no obvious problems, a few have MIS-C (multisystem inflammatory syndrome in children) which can cause permanent heart damage. We haven't fully characterized everything COVID-19 causes.
It's not a disease to catch just to “get it over with.” The more infected people, the more virus copies exist in this world. We saw that the initial disease in China was one particular strain, which was less infectious causing less severe illness. That strain hit the Seattle and California areas back in March. When that strain went to Europe, it mutated and became more infectious. That mutated strain spread throughout New York City in March. New York City hospitals were overrun, while Seattle was able to keep up. That more severe strain won and is now the dominant strain throughout the world. Recently, a new strain was discovered in minks in Denmark. All minks are being culled in Denmark now, but they found 12 humans working on the farms with the mink strain. Scientists are worried that the new mink strain may not respond to the vaccines currently in development. Basically, if we let this virus continue to exist, grow, and mutate, then we will be fighting this for far longer than we must.
The idea of letting the virus run its course while keeping hospitalizations manageable (hammer and the dance) isn't great because unlike some viruses where you usually only catch it once, coronavirus immunity doesn't last very long. Even if you have the disease, you may be susceptible again in 3 months to 2 years. There have been several proven cases where people were sick twice within a few months, from slightly different virus strains. Some of those people had worse disease the second time around. Until we have an effective, long-lasting vaccine, we may just keep passing this around like the common cold, catching it over and over, sometimes with severe consequences.
The vaccine is likely a few months from being approved in the US. Once approved, it will take months for mass production. (For reference, the flu vaccine production takes 6 months, and we've been doing it for years.) After that, it will take months for vaccine distribution. To be protective, we may need two doses, spread 3-8 weeks apart, depending on the manufacturer. Once everyone who wants to be vaccinated is vaccinated (hopefully with 70% compliance and >50% effectiveness), then perhaps we may achieve herd immunity. Note: As of this morning, there is news of a vaccine with 90% efficacy during early analysis in Phase 3 trials. That's fantastic news!
It may take until fall of 2021 before we will be back to “normal.” In this definition of “normal,” we don't have to worry about the little things that may result in an injury that requires going to the ER or urgent care. We can feel confident about going in for a dental cleaning. We can feel safe sending our kids to school. We won't feel guilty about having a loved one in a group care living situation. We can attend big group events. We can travel. We can confidently eat indoors in a restaurant again. Until that time, we have to take this virus more seriously.
Today, we drove to the local shopping district to have some stuff delivered to the trunk of our car, and there were way too many cars in every single parking lot of every single store. The mall parking lot was full. The roads were full. It was like back-to-school shopping or a rainy Saturday afternoon mall event. I'm not sure what's going on inside, but from my vantage point outside of the stores, it didn't look good. Indoor activities with lots of people from outside your household, even if 90% masked, are high-risk situations. I would have thought that the news about the virus surges over the past week would have kept people home. But given the number of cars parked at the mall locally, we will be seeing many more cases in the next few weeks.
As I wrote at the beginning of the outbreak, the epidemic rules for this virus haven't changed. It roughly doubles every week if people do not stick to the rules of social distancing. We are seeing the doubling statistic in various parts of the country, including locally. Experts have written extensively about social distancing, but since you are reading and I have your attention, I will repeat the most important parts here.
- Outdoor interactions are much much safer than indoors interactions.
- Each additional person at an indoor location increases the chances of one person having the virus who can spread it to everyone else.
- Eating at a restaurant indoors or a group exercise class indoors are high-risk activities.
- Masks do a good job of protecting people around you from you.
- Masks do a mediocre job of protecting you. You wear it to show respect to others.
- Sneezing, coughing, shouting, laughing, singing, and eating ejects virus aerosols and droplets.
- Talking normally and breathing doesn't release as many aerosols and droplets with a mask, but viruses can still be released.
- Shared equipment should be decontaminated.
- No physical contact (hugs) with people outside of your small group.
What will I personally be changing for the next few months?
- I will continue to get take out from restaurants that will deliver to my car. However, I will no longer eat uncooked or cold food, like salads. (We have not eaten at a restaurant indoors since March.)
- I will be taking more precautions with handling anything someone else has recently handled, such as my credit card.
- I will continue to go to the grocery store alone, but I will change my clothes upon returning. (I have a toddler who hangs on me.)
- I will no longer shop indoors anywhere (except for grocery shopping). I will just use the curb-side pickup for Walmart, Target, and other such places.
- My family will begin to wear masks when taking walks outside. We want to set a better norm, given the spike in cases.
- We will continue to homeschool, and I will ask our babysitter to read over these precautions as well. (We've already provided her with a variety of face masks to keep her safe, and we've discussed the availability of sick pay.)
For our business, I will be sending out a new company-wide update on the coronavirus. Various situations arose over the past few weeks that affected employees. We've had to set the precedent on how we handle these situations as a company.
AcousticSheep LLC Coronavirus Policy Updates
If you have a household exposure or close contact to someone with COVID-19, you must quarantine for 14 days, according to these CDC guidelines: https://www.cdc.gov/coronavirus/2019-ncov/if-you-are-sick/quarantine.html
If you are sick, please use the guide below.
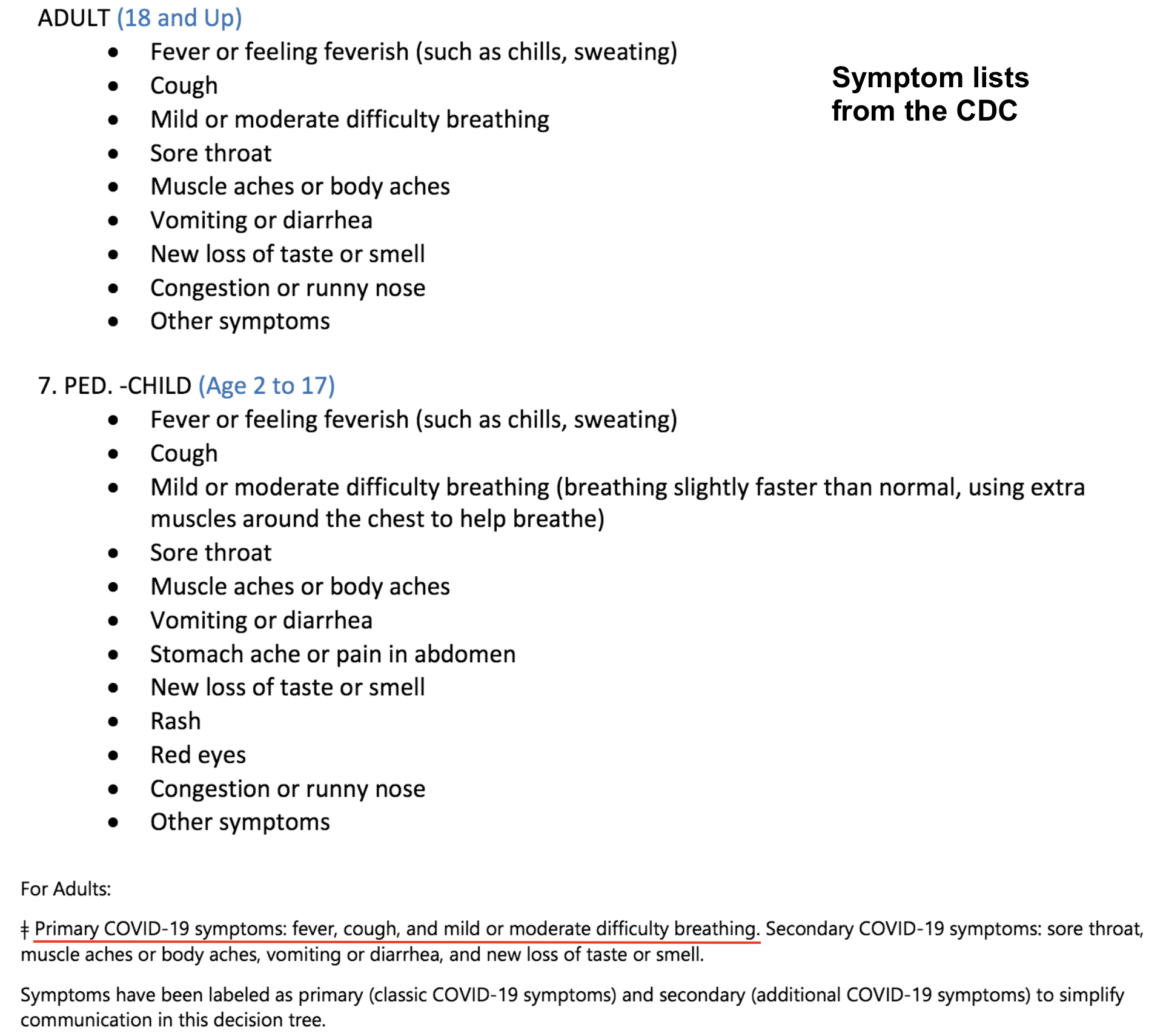
Here are the PRIMARY SYMPTOMS for COVID-19
- Fever or chills
- Cough
- Difficulty breathing
- Loss of taste or smell
Here are the SECONDARY SYMPTOMS for COVID-19.
- Fatigue
- Muscle or body aches
- Headache
- Sore throat
- Congestion or runny nose
- Nausea or vomiting
- Diarrhea
HIGH RISK
Any two primary symptoms
MODERATE RISK
Any one primary symptom or
Two secondary symptoms
LOW RISK
Only one secondary symptom
For example, if you have a cough (1 primary symptom), we consider you to be at moderate risk of having COVID-19. If you have fatigue and a sore throat (2 secondary symptoms), we consider you to be at moderate risk of having COVID-19. If you just have a headache, then you would be low risk. If you started with two symptoms but end up with just one symptom, you would still be considered moderate risk. (You don’t change risk profiles as you get better. Once you are at moderate risk of having COVID-19, you remain at that risk level even as you improve.) We want you to stay home or go home if you are at low, moderate, or high risk for having COVID-19.
If you are low risk for having COVID-19 and do not develop any additional symptoms, you may return to work when you feel better.
If you are at moderate or high risk of having COVID-19, you have three options for returning to work:
- You can get tested and return to work when you get a negative test result.
- You can stay home for 10 days. You can return as long as you’re getting better and no longer need fever-reducing medications. See more detailed information here: https://www.cdc.gov/coronavirus/2019-ncov/if-you-are-sick/end-home-isolation.html
- You can get a doctor’s note saying that you are not infectious with COVID-19 and can return to work safely.
If you develop any symptoms during work, please leave and then let your supervisor know from your car that you aren’t feeling well. For the supervisors, please let HR know about any issues you encounter as soon as possible, as you have done thus far. We will work with you to determine any further actions to make sure we keep everyone safe.
October 28, 2020
I wrote a post on Medium about Travel and Quarantine Between China and Taiwan During COVID-19. It details the experience of one of our supply factory managers, providing insight into a personal experience of how different countries manage the coronavirus pandemic.
April 13, 2020 12 p.m.
Face mask design for people who have beards or wear glasses.
Update from the Shenzhen area of China.
Some factories are up to capacity again. Others are still at about 60% capacity. Schools haven't started for some parts of the country, so parents are still home with their kids. The older grades are going back sooner - April 27 for the Shenzhen area. The younger kids are going back May 11. National testing is being postponed. No school sports or extracurriculars at this time. All school have new entrance and exit procedures to minimize touching common surfaces. All kids are supposed to wear face masks, and the schools are providing them for free.
National parks and community playgrounds are open again. Scenic areas that usually charge visitors are free right now because the government is trying to encourage people to rejoin the economy. Restaurants are allowed to seat people again. Some still have restrictions on the number of people per table and increased distance between tables. Some are less observant of social distancing. Bars and kareoke bars are not open. They tried opening a few movie theatres, but shut them down again. The current congregation limit is 150 people for events like weddings and such. There are no professional sporting events yet. Open-air markets are operating, but people are afraid to go to those. Many people are still ordering groceries online and getting it delivered for the convenience. Most people are still wearing masks, though a few have started to not wear masks.
Some businesses did not make it through the epidemic, so some workers are out of jobs. Meanwhile, some workers are still at home with their kids. So there is some mismatch of resources. The travel industry was hit hard. Airlines are struggling. Hotels seem okay because many people are using them for quarantine, especially international travelers who are required to be quarantined for 14 days. Pockets of infection are being found, mostly in areas that cater to international travelers. (Note that this is from the Chinese press.) Businesses are now worried about the global recession and cancelled orders from international customers.
No magic treatments have been found. Everyone is just waiting for the vaccine for life to return to normal. There is hope that the new antibody test will help with figuring out the rate of asymptomatic infections.
Question: Do you think the immune response could be part of onset of pneumonia? That's my concern is that if you get infected a second time the next the immune response could cause more severe symptoms? It happened with H1N1 when young people had a more aggressive immune response they got fluid filled lungs?
Answer: Sounds like you are referring to the cytokine storm. So in an effort to fight off the virus, lots of markers called complement attach to the viruses. These markers tell the other immune cells what to kill. But because there is so much virus, the mounted immune response is so aggressive, that there's too much collateral damage, like to lung tissue. The other immune cells come over and set off hand grenades where they are told, and while it destroys virus, it also destroys the lungs, liver, endothelium (lining of blood vessels), and even the heart. So in theory, an overly-aggressive immune system can cause rapid decline is otherwise healthy patients. But whether someone has a "good immune system" or not doesn't seem to correlate with why they may exhibit this over-reaction. Eventually, someone might find a few reasons, but right now, there's no way to predict. Typical immunosuppressants like prednisone have been tried and don't improve outcome. Also, nothing's ever cut and dry in medicine. While a cytokine storm may be the pathophysiology for some people, it's just one of many reasons for the rapid decompensation. We know for sure the virus attacks lungs, liver, heart, and endothelium. Probably other organs, specific tissues, and possibly specific cells too. The stuff about it attacking red blood cells and affecting heme porphyrins is being debunked. That didn't make much sense to begin with.
As for catching it a second time, no, I don't think it would make things worse. And I don't think you would catch it again anytime soon. We would make enough IgG with the first go around to not catch it again for a few years at the minimum. Immunity may wear off, but would take years. The whole thing about "catching it again" has more to do with false negatives on the test than anything else. Viral shedding from the nasopharynx can last for weeks after recovery from illness. Nothing too surprising. And can a few people recover and then get worse again? There are always exceptions. Focusing on the outliers misses the point. (Scientific discoveries, however, are often made by looking at outliers, so it's still important for scientists to look at) But for the general public, talk about the exceptions is more about drumming up fear or just incompetent reporting because they don't understand the science or basic stats with testing error. (Remember the PCR has >25% false negative rate!)
April 3, 2020 12 a.m.
Question: Surgical masks when out on a walk—yes or no? When grocery shopping?
Answer: Yes.
We were out today because our printer broke. The sales people came way too close, and it was hard to avoid them talking in my face. I was getting pretty uncomfortable because they didn't keep their distance. I'd say go ahead and wear a mask. It might not help you 100%, but it can help. Plus, we just need to set a new norm. That way, the salespeople can wear masks too without feeling awkward. With the percentage of people possibly walking around pre-symptomatic, I don't feel safe anymore.
If I wish everyone around me would wear masks, that means that I should wear one too.
Are there enough masks to go around?
Front line healthcare workers should have the priority for getting personal protective equipment. But there is a shortage. The sentiment in a Facebook Group for doctors is that doctors are getting more and more desperate for proper equipment. We know now that it's basically airborne. If someone with COVID-19 talks in your direction, virus is traveling toward you. Patients are presenting to the ER not just with the classic respiratory symptoms but with a variety of heart problems, delerium, and various other non-respiratory complaints, only to be later diagnosed with the coronavirus. Anyone in a hospital or even urgent care should probably be properly protected now, with N95 masks and other gear. But there just aren't enough. Or is there enough?
- Did you know that the government has not yet set a fixed price on critical pieces of equipment? New York is paying $7.50 per N95 mask. They are normally $1.45 per piece. In fact, all protective equipment, ventilators, medications, etc. are way overpriced now. We are letting opportunists price gauge hospitals and state governments. This needs to stop. We need to have a standard price for the nation for this period of time. Price-fixing for national security is not new, and it does not mean a "slippery slope" to whatever. We are fighting a war with a germ, not each other. Let's focus on fighting the right enemy. Pricing will eventually be fixed for the equipment, because it's the obvious thing to do. When the media pushes the issue out there, public sentiment will agree that it's the right thing to do temporarily. I just wish it was done 3 months ago when everyone bought out the N95 supply from the standard distributors like McKesson. We knew they were going to sell out, we knew there would be a price war, we should have controlled pricing months ago.
- Did you know that the government has not yet banned exports of masks and other essential equipment? If someone in Saudi Arabia wanted to buy N95 masks for $10 apiece, a distributor in the US can ship masks out of this country to the highest bidder? Nearly all other governments around the world have stopped the export of essential equipment. We are abandoning our own doctors, potentially killing them and the people that they would have cared for, just so some middle man can make a few dollars. We have to stop exporting the supplies we have. It's ridiculous that doctors are literally sewing their own masks while masks are being exported.
- Did you know that we still had a 7.5% tariff on essential equipment like face masks and gloves left over from the trade war with China until March 7th? On March 7th, 16 people had died in Seattle, and Italy was preparing for lock down of the Lombardy region. Remember- a tariff is a tax our own government levies on the American companies importing from overseas. It does not punish the overseas supplier. The money is paid by the importer- the American company.
In late January, China was desperate for personal protective equipment like face masks. Then Europe started selling out of hand sanitizer in early February. These are things even I saw coming. If our public health system was in any way prepared, we would have seen this coming. We would have put in place export bans, fix prices, cleared tariffs, increased hand sanitizer production, and encouraged stockpiling for our own country. It's like stocking up on toilet paper. The later you recognized the problem and decided to go to the store, the less likely you would get the brand you want, at the price you want (the 36 double packs, not the tiny 4-packs). Our public health system should have seen this coming, gauged what we needed, and hoarded stuff for our own country before the rest of the world jumped in to compete for limited supplies. In mid-February when it became obvious that the coronavirus had escaped China and was starting to take a foothold in Iran, a country that could not control a disease so contagious, we should have known that it was coming and started prepping as a country.
It's disturbing to me how many things should have happened but didn't or finally happened too late. So now I am contributing to the conversation for what I think should happen going forward. We need widespread testing. We need to strictly quarantine the sick. We need to trace the contacts. We need to quarantine them. We need to keep up with domestic and international travel restrictions. (The President has already said for anyone traveling out of New York City to self-quarantine for 14 days. We need to do that immediately for New Orleans. And then next week, we will be adding five more cities to the list.) If we do those steps, we will get this under control and be able to lift the stay-at-home order for most of the country to get people back to work. The only way we will come out of this with an intact economy is if we get really serious about quarantining the sick and their contacts. We must completely suppress the disease. If we get serious, we can get back to work in 3 months. If we keep this rolling half-closure, self-quarantine but keep your privacy and no contact tracing nonsense, we will not get back to work until the vaccine arrives- in 18 months. I've written to my Congressman and Senators. We need to throw money and manpower at public health. It's far cheaper than endless stimulus packages and will pay dividends.
The other thing we need to do is to evaluate what shortages will arise when other countries close their borders to deal with the crisis. I am not en economist, and I don't know what is produced where in the world. If there are things we depend on from third-world countries, we need to prepare ASAP. Perhaps it's coffee beans, chocolate, vanilla, rubber, or coconuts (and coconut derivatives). I don't actually know. Something to think about.
April 2, 2020 11 a.m.
I posted some long-form pieces on Medium recently. Here they are.
How and When We Will Get to the New Normal
Coronavirus Can Be Ronald Reagan's Alien Invasion
Coronavirus Quarantine Application Specifications
Common Problems Leading to Inaccurate Coronavirus Mortality Rates
I've changed my mind on a few things based on new findings and research.
- Masks. The CDC and federal government is debating over mask recommendations. I had initially thought that masks were overrated, and when the coronavirus was first starting out, they were. Now that we have had a really hard time getting this outbreak under control, there are enough people walking around not knowing they are infectious that masks may be a good idea now. The idea is still the same- masks mostly protect people around the person wearing the mask, not the other way around. That's why for some time in Asia, people were being fined for not wearing a mask. The goal was to prevent the unknowingly sick from spreading disease.
-
China Numbers. I guess I was perhaps naive to think that the WHO was a trustworthy organization. There are some serious reasons to think that they are either unable to unwilling to stand up to China's bullying. Perhaps to gain access to information, they have had to compromise their objectivity. Or perhaps they are more seriously compromised. The Joint Mission report between the China CDC and the WHO released in February was the most comprehensive information we had at the time, and nearly everyone referenced information in that article. But some things don't add up.
- The number of urns delivered to Wuhan in recent weeks - 42,000 - is many times the number of officially reported deaths at 2,535.
- China has long bullied Taiwan, claiming that Taiwan is part of China, and forcing Taiwan's exclusion from the UN, WHO, and many other international organizations. In this video, a senior WHO official can't even say the word "Taiwan." First he pretends to not hear, then he hangs up, then he evades the question. If China controls the WHO to this extent, then WHO has no power and therefore no credibility when they supposedly report numbers from China.
- There is also speculation that the number of cell phones deactivated - 15 million - in recent weeks may indicate deaths, though there are many reasons why cell phones may have been deactivated.
March 22, 2020 1 a.m.
You may have heard about how you shouldn't use ibuprofen to treat the fever with COVID-19. Instead, you should use Tylenol or paracetamol (Tylenol equivalent in most other countries about the world). This is based on theory of how ibuprofen impacts an enzyme's activity. However, we are all grasping at potential marginal benefits here, so if there is a theory that shows something might make a difference, some people are going to act on it. Apparently, there are some prominent scientists promoting this idea, and it was somehow attributed to the World Health Organization, which I take seriously. Officially, however, the WHO released a statement on March 18 disavowing this idea. The human body is an extremely complex system. A recommendation for avoiding ibuprofen cannot be made based on theory. It has to go through human trials. But I would concede that this is an easy change, so just take Tylenol first. If you really prefer ibuprofen, then just take it. Don't worry too much.
You may have heard about hydroxychloroquine or chloroquine, with and without azithromycin, as a cure. This poorly designed and executed "study" was announced on Tucker Carlson's FOX news show. If you watch it, the lawyer representing the scientists is so sketchy even Tucker had a hard time believing what he was saying. This WIRED article breaks down what happened and hints at the potential motivations of the people involved with promoting chloroquine. My personal view after reading about what happened in the experiment is that it's unlikely the drug has a significant effect. And whatever effect it does have, it makes up for it in side effects. It's not a benign medication. Many people will experience at least mild side effects. China is doing clinical trials already, and it seems that the U.S. may as well. If it seems to help, then the people who have COVID-19 should have first dibs in trying it, which is happening at some West Coast hospitals already. As a prophylactic (preventative) medication, I cannot recommend it at this time. For prevention, we would have to give it to lots of people, and many of those people would have bad side effects, some so serious medical attention is required. There is a saying that "the cure is worse than the disease." In this case, the prevention is worse than the disease.
It is important to watch out for scams when we are all anxious and wanting to believe in positive news. It's equally important to watch for scammers feeding off people wanting to do good and contribute to this situation. Shady characters come out during times of crisis, feeding off our anxiety. They tend to promise too much, and they look for trusting victims.
In good news, Elon Musk has committed Tesla factories to producing ventilators and N95 masks now. While Elon tends to run late with his projections, when he says he will do something, it gets done. Of all of the silicon valley giants, he actually manufactures in the US and makes real, physical things here, not overseas. His efforts will help quite a bit!
You may have heard about a report from the Imperial College of London that models various scenarios, all quite pessimistic. I think the main takeaway from the modeling is that if we don't do anything, the results are catastrophic. If we do a lot, as early as possible, then we can control the spread of the disease to make it more managable. In reading through the report, I don't entirely agree with all of the inputs to their model. Some things are up for debate, such as doubling time or mortality rate. But the one input that I found most troubling is how they use flu transmission to model spread among school kids. Kids get the flu, and they transmit the flu by coughing in their friend's faces and via fomites (toys, doorknobs, playground equipment, etc.). With the coronavirus, it seems that kids don't transmit as readily. They don't test positive as much as they should. The test is a nose and throat swab that looks for virus parts (RNA via PCR). Kids tend to test negative, which means there is not enough virus to spread disease when they cough. So when this report uses flu transmission in schools as a model for how coronavirus spreads in schools, I have to wonder if they are using the best inputs for their model.
March 21, 2020 11 p.m.
Eight days ago was the last day of school in Pennsylvania. Four days ago, Pennsylvania declared all non-essential businesses to stop operations, particularly public-facing businesses. We handed out laptops Monday afternoon to everyone whose job duties allowed them to work from home. Two days ago, it expanded to all non-life-sustaining businesses. A new list of allowed businesses were handed out. As electronics wholesalers and e-commerce distributors, our warehouse and e-commerce shipping component is considered life-sustaining business. We are very fortunate to be able to continue operations. However, because we want to do our part in flattening the curve and minimizing risk all around, we are allowing only one person at a time in our warehouse, with strict cleaning at the end of each shift.
- Monday - shipping online e-commerce orders
- Tuesday - shipping wholesale orders
- Wednesday - complete disinfection
- Thursday - shipping online e-commerce orders
- Friday - processing returns, exchanges, and warranty claims
We have written down what we are doing to protect our customers during these extraordinary times. We are closely following all federal and state developments and recommendations to make sure we protect our employees while serving our customers. As an MD and wannabe epidemiologist, I am in particular keeping my ear close to the ground for new scientific announcements and participating in a physician group to understand what's happening in medical circles.
March 14, 2020 2 a.m.
Testing for the coronavirus, while being ramped up, is still not widespread. Results still take a day. At this time, only the hospitalized patients get on the list for testing. Therefore, we are missing many cases in the community. However, it is important for many people (school officials, event planners, managers) to know approximately how many cases may be in a community. With that information, they can make better plans.
Also, we are still dialing in the doubling time for the US, what the mortality rate is, and what the clinical course looks like. Based on the information out of China, South Korea, and some anecdotal information from Seattle doctors, we are looking at something around these numbers.
- Doubling time: 7 days
- Mortality rate: 1.5%
- Hospitalization rate: 20%
- Number of days from infection to death: 20
- Number of days from infection to hospitalization: 12 days
- Number of days from infection to being out of the hospital, if hospitalized: 40
In medicine, we typically go with a 95% chance rule. If something is 95% likely to be correct, then we decide to believe that it's correct. And we make decisions on that 95% chance all of the time. In theory, one in twenty decisions will be wrong, but we just take that risk.
To help everyone make their own models for how many cases of the COVID-19 might be in their community, I put together a spreadsheet that will do a lot of the epidemiological calculations automatically. In the yellow fields, you can enter your guess for the mortality rate, doubling time, or any of the items in the list above. I've pre-filled it based on my guesses. Don't make any changes to the fields below that. They do the calulations.
Look to the right for the orange-labelled chart with the final rounded calculations. Let's say your local hospital just confirmed 2 cases of the Coronavirus. Look for the first day that there would be 2 cases in the hospital. With my projections, it would be Day 37. On Day 37, there would be an estimated 35 cases in the community. 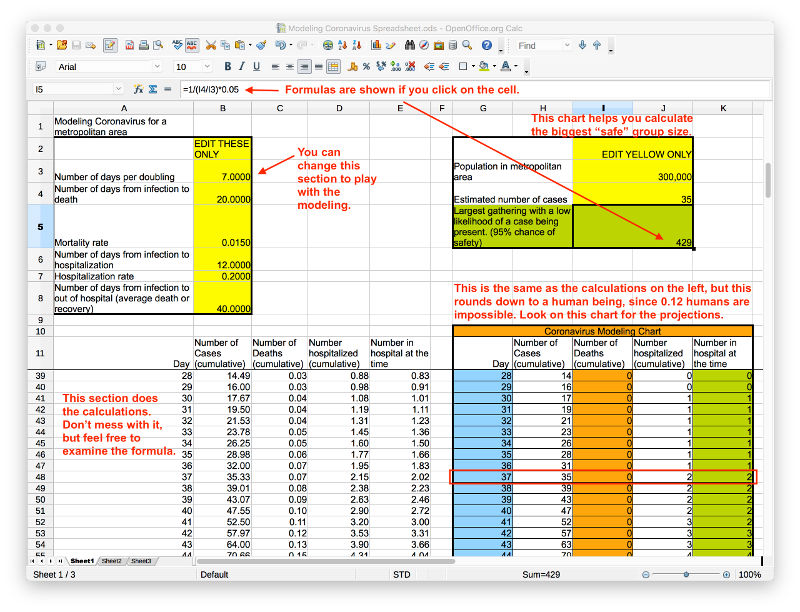
I have a second, much simpler tool on the top right. Fill in your local population and how many estimated cases are in your community. The calculator will then tell you that there's a 95% chance you won't encounter someone with the coronavirus in a group of a certain size. We have about 300,000 people in our greater "metropolitan" area. Rumor is that we may have seen 2 cases in our local hospitals. I fill in that we have 35 cases in our community. The tool tells me that if there was a group of 429 people, say at a school, there's a 95% chance that no one has the coronavirus. So for a small school, I'd feel pretty comfortable going there.
When we see our first death, however, there would be 511 cases in our community. At that point, I would only feel relatively safe having contact with 29 people or less.
March 11, 2020 11 a.m.
Question: If quarantine successfully slows/stop the virus spread, what prevents continued transmission when people resume normal activity?
Answer: When people resume activities, they will take a bit of time to readjust. And the resumption may come in phases. Perhaps we allow travel again, or perhaps schools start up again. When each phase seems safe, then we can lift another restriction in 1-2 weeks. If people get sick again, then we would have to go back. In China, they have gradually allowed people to come back to work. A few weeks ago, the government allowed 30% of workers to return. Then when that was safe, they allowed more. Flights have resumed as well there, but the temperature scanning continues, and they've implemented controls to prevent people from bringing the virus back in from high-risk countries. It won't be an all-or-nothing scenario. We've already started aspects of social distancing like discouraging travel and cruise ships. It's a long continuum of ideas we can implement. The sooner we start the easiest aspects of it, the less we'll have to suffer later. Hopefully everyone will continue to keep up excellent hygiene habits after this too, and we may end up with fewer colds in the future!
March 11, 2020 3:00 a.m.
Here are AcousticSheep, we are taking the necessary steps to protect lives in our community and yours. By doing everything we can to stay healthy, we aim to never spread the Coronavirus to venerable populations locally or in the mail. A potential customer asked yesterday if it was safe to order from us. In my opinion, ordering from us is as safe as it gets. Some large online shopping companies may have warehouse workers who come in sick because they won't get paid otherwise, or are even fired for being sick or injured. Our last component stock from China was placed on a ship prior to the outbreak. It naturally decontaminated during the 6 week journey and arrived here in late February. We quality control everything in the US, and we do the final assembly and packaging here in Erie. Unlike our knockoffs on Amazon, we ship from Erie, PA not another country. We have seen zero cases locally.
In preparation for Coronavirus arrival to our area, here are the steps we are taking.
- Set up work-from-home for office employees when the Coronavirus arrives.
- Discuss contingency plans for employees whose job duties require in-person presence, including staggered work hours to minimize interactions.
- Quarantine all incoming products (domestic and international suppliers, customer returns) for 5 days of natural decontamination. It has been shown that the virus is undetectable after 5 days on most surfaces.
- Advise employees to stop all hand shaking or hugging with vendors, customers, or anyone who comes to visit.
- Provide ample access to hand sanitizer and hand washing facilities.
- Recommend cleaning employee's personal work area 1-2 times per shift.
- Institute a new disinfecting (more than just cleaning) plan involving a checklist of over 50 items daily. Other items weekly.
- Track all employee travel, including domestic car travel outside of Erie.
- Discourage non-essential travel and large gatherings.
- Prohibit coming to work when ill (consequences are formal insubordination write up or worse).
- Give more PTO to cover minor illness than our 30-day PTO policy.
- Reassure that time needed for self-quarantine will be supported by the company.
- Encourage compliance with social distancing measures at work and personal interactions.
- Educate employees about basic Coronavirus facts and how to monitor for symptoms.
- Open lines of communication for concerns and questions.
- Update employees regularly.
Here are some parts of my letter to all AcousticSheep employees.
As the Coronavirus pandemic makes its way through the U.S., we anticipate some disruption of work at some point in the next 1-2 months. The timing depends largely on when the transmission rates are decreased by canceling large events, discouraging travel, and the precautions every person takes. The sooner we implement the less disruptive elements of social distancing as a nation, the slower the disease will spread. If we wait too long, the quarantines would have to be more stringent and more people will die. This is happening in Italy. On-the-ground reports from doctors on the West Coast are also starting to sound pretty desperate. There are 12 presumptive cases in PA, all on the Eastern side of the Commonwealth. There is no data on how many tests have been done.
As I detailed in my Coronavirus post and as the news media has started to teach, the key here is to "flatten the curve" to reduce excess mortality. If we do nothing, then the hospitalizations required will grossly overwhelm our medical system, and many more people would die, even people who do not have the Coronavirus. If we all take actions to slow down the spread, then people who need oxygen or machine ventilators will be able to get it for 2-4 weeks, recover, and leave the hospital for the next set of people who need the equipment.
Some of the actions are up to businesses and corporations. Here are the things we are doing for this epidemic... (highlighted above)
These policies may change over time as the situation changes in our area. Thank you for your contributions, and let's all stay healthy to keep our community healthy with good access to non-overwhelmed medical care.
Symptoms of COVID-19 are as follows:
- Fever
- Cough
- Aches and pains in muscles and joints
- Fatigue
- Productive cough (mucus)
- There may be some nasal congestion or runny nose, but this is actually not common for this illness.
Worsening of symptoms almost always involves feeling short of breath. According to the most recent reports in the US, the incubation period averages 5 days. Symptoms may be mild to moderate for a week. After that, most people slowly recover. Some make a turn for the worse and start to feel short of breath. When that happens, it's time to go to the hospital for oxygen.
You should call your doctor to let them know about your symptoms. Do not just show up. And definitely don't just show up to the ER if you are not gravely ill. Call ahead, and ask if they have test kits. If you are diagnosed with COVID-19, follow instructions from your doctor. Keep us (supervisor and HR) informed every 1-2 days of how you are doing. Hopefully testing will become more readily available so you can know for sure whether you can return to work or not if it turns out to be just a cold. (Try to not catch colds because it's just a huge hassle given the situation, potential confusion with COVID-19, and quarantine requirements if we don't know for sure!)
If you come into contact with someone who is diagnosed with COVID-19, you should let your supervisor and HR know. We would walk through the CDC's risk assessment to determine what the next steps should be. The Pennsylvania Coronavirus hotline is 1-877-PA-HEALTH (1-877-724-3258) The current self-quarantine time period is 2 weeks because it can sometimes take that long for illness to show up.
March 9, 2020 11:00 a.m.
I live in the suburbs of a medium sized city in Northwestern Pennsylvania called Erie. It's the fourth largest city with almost 100,000 people. The "metropolitan" (if you can call it that) area is about 300,000 people covering 800 square miles. We draw workers from the entire county and a few surrounding rural counties.
We don't have a subway, though we do have an Amtrak stop. We have a Greyhound station and a local bus system. We have a small airport with 7 gates, but only 3 are used regularly. We only fly to the hubs Detroit, Charlotte, and Chicago. Many people decide to fly out from our surrounding bigger cities including Cleveland (2 hours drive), Pittsburgh (2 hours drive), Buffalo (2 hours drive), and even Toronto (3.5 hours drive).
We are small enough that we don't really have traffic jams. We have minor league baseball, basketball, and hockey teams. Pretty much every working person has a car because there is really no other way to get around, especially in the winter when we get a lot of snow.
We have 3 major hospitals locally. UPMC is our level II trauma hospital with 423 beds. St. Vincent has 413 beds, and Millcreek Community has 167 beds, for a total of 1003 beds. UPMC Hamot reports an average census of 400, meaning they only have 23 unused beds normally. The marketing department tells me that they have plans for opening up floors and wings for overflow if necessary. They have 56 critical care beds. I will assume that we have 250 available hospital beds by opening temporary overflow portions of the three hospitals.
The current estimate is that the number of cases double each week. If we do nothing for social distancing (quarantine), 10 people hospitalized this week mean 10 more people hospitalized next week. And then 20 more the week after that. Week after that, 40 more. Each person stays in the hospital for 3-6 weeks. (In my estimates, I will use 4 weeks.) It takes a person about seven days to progress from infection to hospitalization.
We can slow down the spread of the virus with a soft quarantine like what Italy is doing. It's less disruptive economically than shutting down all businesses and will still work to slow down spread. Italy has imposed quarantine measures for 16 million people by shutting down gyms, pools, museums, and ski resorts. Weddings, funerals, and sport competitions are suspended, and people are told to stay home as much as possible. Restaurants can open between certain hours, but customers must sit at least a meter (a little more than a yard) apart. These measures would result in a gradual decline in new cases.
When an infectious disease takes hold of an area, the progression in disease spread is quite predictable because it usually follows mathematical principles. Instead of doubling every seven days as one might expect in a large city, I will estimate that doubling takes 10 days in our area. Based on that model, here are some key takeaways.
- When we see our first death from the Coronavirus, it would be four weeks until our hospitals reach capacity, assuming the hospitals open all available temporary overflow space.
- When we see four deaths from the Coronavirus, we would have one week until our hospitals reach capacity. There is a one week lag time between when we start social distancing to when our new hospital cases begin to slow down.
- If we implement Italy-style social distancing at two deaths, we may be able to keep our hospitals from exceeding capacity.
- This assumes that we catch all deaths caused by the Coronavirus. Some mortality may be hidden by other problems, so we have to be vigilent.
I think that if we begin to ban certain mass gatherings when we reach two deaths, we may be able to slow down spread enough to prevent from having to also shut down schools. If we waited until four deaths to do anything, then we would have to take more drastic measures to prevent running out of hospital space. These are optimistic predictions. We do have a slightly older population with health issues. The problem with running out of hospital beds is that some people won't be able to get oxygen and will die from that. This is called excess mortality - where normally someone wouldn't die if they had routine access to medical care.
If I am less optimistic, then we have 100 extra beds, and the doubling time remains seven days. In this case, as soon as we detect our first death, many things should be shut down, including schools and some types of businesses that involve large crowds. It seems that I've been too optimistic so far, so this is the more likely scenario. This does not change the fact that we should all be prepared to stay at home for a few weeks and maintain sanitary procedures (frequent hand washing, staying home when sick).
March 7, 2020 1:00 p.m.
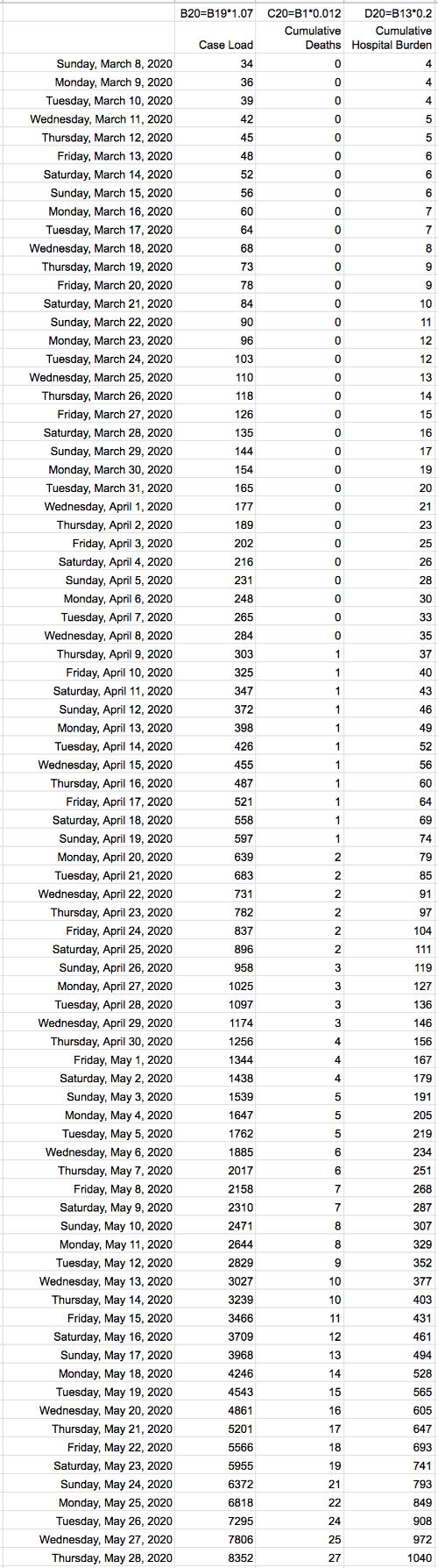
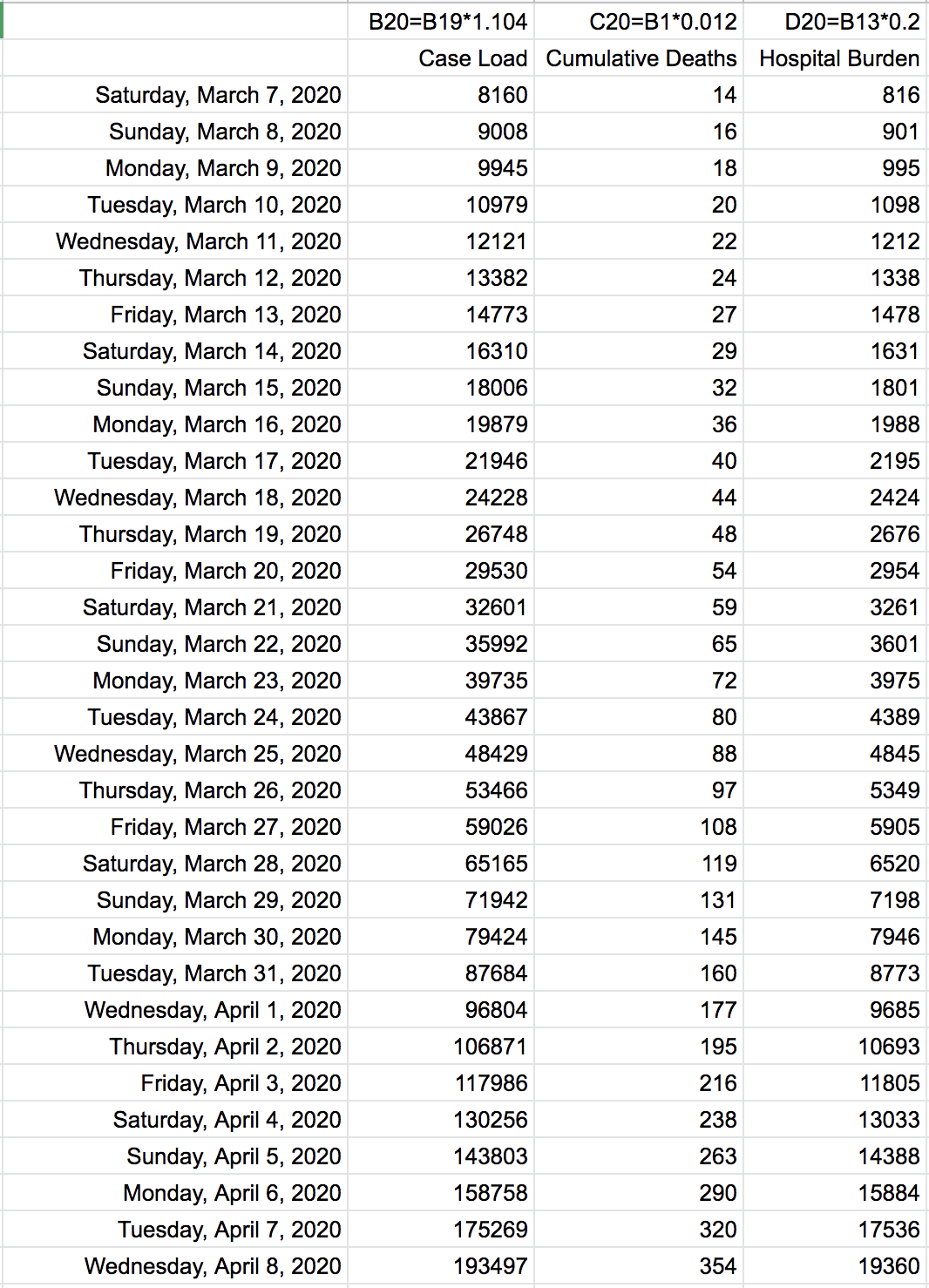
As of right now, there are 15 deaths in the Seattle metropolitan area. According to mathematical models based on cases doubling every 7 days and 20 days from infection to death, there would be about 9000 infected people in the Seattle area. Here is an updated chart that depicts what we are looking at for Seattle if they do not start social distancing measures such as closing schools and banning large gatherings. Case load doubles every 7 days in the second column. The third column shows a death rate of 1.2% with a 20 day off-set because I estimate it takes about 20 days for someone to die from the date of infection. The fourth column shows how 20% of people will need hospitalization (or at least supplemental oxygen) with a 7 day off-set because it typically takes 7 days from the date of infection to get bad enough to go to the hospital for oxygen.
According to the February 28, 2020 Joint Mission WHO-China report based on data from China (which is actually very good - remove your biases and read the report if you care to), the symptoms are as follows:
- 87.9% fever
- 67.5% dry cough
- 38.1% fatigue
- 33.4% sputum production
- 18.6% shortness of breath
- 13.9% sore throat
- 13.6% headache
- 14.8% myalgia or arthralgia (bodyaches)
- 11.4% chills
- 5.0% nausea or vomiting
- 4.8% nasal congestion
- 3.7% diarrhea
- 0.9% hemoptysis (coughing blood)
- 0.8% conjunctival congestion (pink eye)
On average, respiratory symptoms like coughing and fever begin 5-6 days after infection, with a range of 1-14 days. 80% have mild to moderate disease which do not require hospitalization. 13.8% have severe disease requiring hospitalization and supportive care like supplemental oxygen, IV fluids, and supportive medications. 6.1% have critical disease where one or more organ systems fail. According to the report, most people end up having symptoms of some sort. It's rare for someone to have caught it but not show any symptoms at all. However, I have to add that we (Singapore) only developed serologic testing (blood testing for antibodies against the virus) in this past week, so our ability to find asymptomatic cases was limited, and the information available when the report was written was probably not enough to draw the conclusion that asymptomatic cases are rare.
According to the report, "the median time from onset to clinical recovery for mild cases is approximately 2 weeks and is 3-6 weeks for patients with severe or critical disease. Preliminary data suggests that the time period from onset to the development of severe disease, including hypoxia (low blood oxygen levels), is 1 week. Among patients who have died, the time from symptom onset to outcome ranges from 2-8 weeks."
I think one important thing to point out here is that this differs from a cold in that Coronavirus disease has very little stuffy or runny nose (5%) and almost always a fever (90%). If you have a runny nose with no or low fever, you most likely have a cold and do not need to be tested for Coronavirus.
Based on the assumptions for mathematical modeling of the exponential spread in major cities, here is a quick and dirty way to estimate current infected cases based on confirmed deaths in a metropolitan area. The reason why this is necessary is because we aren't testing enough people to actually know how many people are infected. We have prioritized testing the sickest people, so we will at least detect the deaths. We have to extrapolate from deaths to number of people infected.
Number of people infected = (deaths * 83.33) * 1.104 ^ 20
Where 83.33 = 1 / 0.012 (using 1.2% as the estimated mortality rate), 1.104 ^ 7 (latest doubling estimate 7 days) = 2 (double), 20 days from infection to death.
My feeling now is that the hospital burden doesn't seem as high as it should be according to the mathematical model. The hospitals in the Seattle area should have seen a 10-20% increase in patients and should be approaching capacity by mid-late March. Maybe they are starting to be stressed but we haven't heard about it yet because there is bigger news coming out from there, such as the number of deaths. Plus, they don't want to cause panic. Or it could be that my 1.2% mortality is low. I'll have to re-run the numbers once more information is released around the world.
March 6, 2020 1:00 p.m.
Question: Why do you think that the vast majority of the cases are ages 50-59? Why not large numbers over 50 also, if they're more at risk for worse disease?
Answer: This is a great question. There are a few reasons why the many cases are ages 50-59. First, a large portion of Chinese are that age to begin with. As you may have heard, China went through a period of high population growth and then experienced a famine. The government then stepped in to control the growth by implementing the one-child policy, which spanned from the 1980s to 2016. That caused artificial pressure on the demographics of the country, which looks like this.

The second reason is that they are most likely to be tested. They are still working, having to buy food for the family at home, and simply most active in society. As they leave their buildings, they are scanned for a fever. If they have a fever, then they are tested. Families in China live in extended family structures more than in the US. There is often a set of grandparents helping to watch the children while the parents work. They all live together in one household.
The other major thing people have talked about is how there are more males than females who died, leading to some speculation that it's due to more males being smokers. Again, you have to look at the denominator, which is how many people were male to begin with. The one-child policy put a lot of pressure for families who wanted the preserve the "family name" to have a male heir. The are 1.15 males per 1 female in China right now. I think that's one of the reasons for why more males died- there are simply more males.
UPDATE 3/8/20: Per the WHO-China Joint Mission report, males did die at a higher rate than females, not just in gross numbers but in percentage of deaths per infected person. Case fatality rate for males was 4.7% and females was 2.8%. So indeed, lifestyle choices such as smoking and alcohol do affect general health and therefore mortality rate.
Question: Regarding the chart of predictions on case # and deaths through the next few months, is that based upon ONE focal point, like a person in California, causing up to 37000 deaths? Is that nationwide with all the multiple clusters? And we are already at 11 deaths in the US, so if this is based on one person, what does the actual death rate look like nationwide?
Answer: I partially answered this question on the March 3, 4:30 p.m. update. It's per metropolitan area, but I don't think we will get to 37,000 deaths from one focal point. I feel like the tipping point for action is probably 10-20 deaths in an area (like what we are seeing in Washington State) before people are scared enough to take real action. That means there would be about 10,000 people infected in an area when we start to quarantine. (I have to update my timeline again, but we're looking at the end of March according to the chart I posted on Feb. 29.) The quarantine will cut down on transmission rates tremendously. But there is a 20 day lag until people actually die. (Around April 19 per the chart below.) So if "social distancing" is implemented at 20 deaths, 20 days later, we would see deaths from the 10,000 people who were infected at the time when we finally took decisive action. 20 days later means about 150 people would die ultimately. And at least 500 people would be hospitalized for 1-3 weeks. I think that the health systems in Seattle would be stressed with 500 extra patients. That's if we were really strict with social distancing, which is nearly impossible. So probably more than 500 would be hospitalized and more than 150 would die in Seattle.
People are saying that because South Korea currently has 42 deaths out of 6593 confirmed cases that the mortality rate is actually 0.6%. They are failing to account for the 20 day lag in deaths. Lag time is important! We won't know the true mortality rate until at least 30 days later (in some cases, 2 months) when most people who would recover have done so. Plus, South Korea is doing a ton of testing. Testing is free, it's at a drive-thru, it's quick (a few hours), and there is no shortage of tests. So if you test a lot of people, you will find many more non-serious cases. My guess is that the true mortality rate is probably just under 1%, which is still 10 times more deadly than the flu.)
My gut feeling is that there were more Coronavirus deaths in Seattle than what's been reported because we are still limited in our ability to test. I continue to read many stories from people who are surely high risk but being denied testing due to a shortage of tests even yesterday and today. They went back and found 2 more Coronavirus deaths before the first reported death on February 29. (I'm not sure how they figured that out on dead bodies... I'm not sure I want to know.) Seattle is an unfortunate guinea pig for how and when we will respond when it hits our communities.
In other news...
There is clearly a very large cluster in Seattle causing many deaths because it found its way into a nursing home and a hospital. Another cluster is currently being investigated in Westchester County, one of the wealthy suburbs of NYC.
Since we don't know how many tests have been performed and where, we can't be certain that there aren't other clusters yet undiscovered. It's been a slow ramp up, but hopefully by next week, we will be able to test everyone who is hospitalized with Coronavirus symptoms. It will probably take until mid to late March to have the infrastructure in place to test everyone going to the doctor. Actually, I hope we won't be telling people to physically go see their doctor. Other methods for outpatient (non-serious, mild) doctor visits should be made available.
China now has a 15-minute test running at the airports. They report detecting a positive test in 1% of incoming travelers. 1%! That's crazy. Hopefully the test just has a high false positive rate. UPDATE March 9, 2020: I spoke with our China contacts, and indeed, this is available at the Shanghai airport. It's not very accurate, but it allows for quick screening for triage purposes. They can quickly isolate someone for further testing. They are using this screen for incoming travelers from high-risk countries like South Korea or Italy. That explains the high percentage of positives. In fact, 10% of people from Iran is testing positive according to the Chinese media.
March 4, 2020 4:30 p.m.
The CDC has changed the way they report again. Most states are now allowed to test, since the FDA finally loosened their restrictions. The states supposedly have test kits as of today, but there are still many health professionals complaining about either not being allowed to test or not having any test kits. The CDC won't report the denominator (how many people were tested) still, claiming that, "Now that states are testing and reporting their own results, CDC's numbers are not representative all of testing being done nationwide." So for those of us trying to gather information to make informed decisions, this makes our work harder.
But not to despair, there are lots of people who are taking it upon themselves to crowdsource data. The Johns Hopkins map was famous after our HHS acting deputy secretary asked if it was still working on Twitter. There is a 17-year-old in Seattle who had the foresight to start a website collecting routine scrapes of charts from around the world back in January.
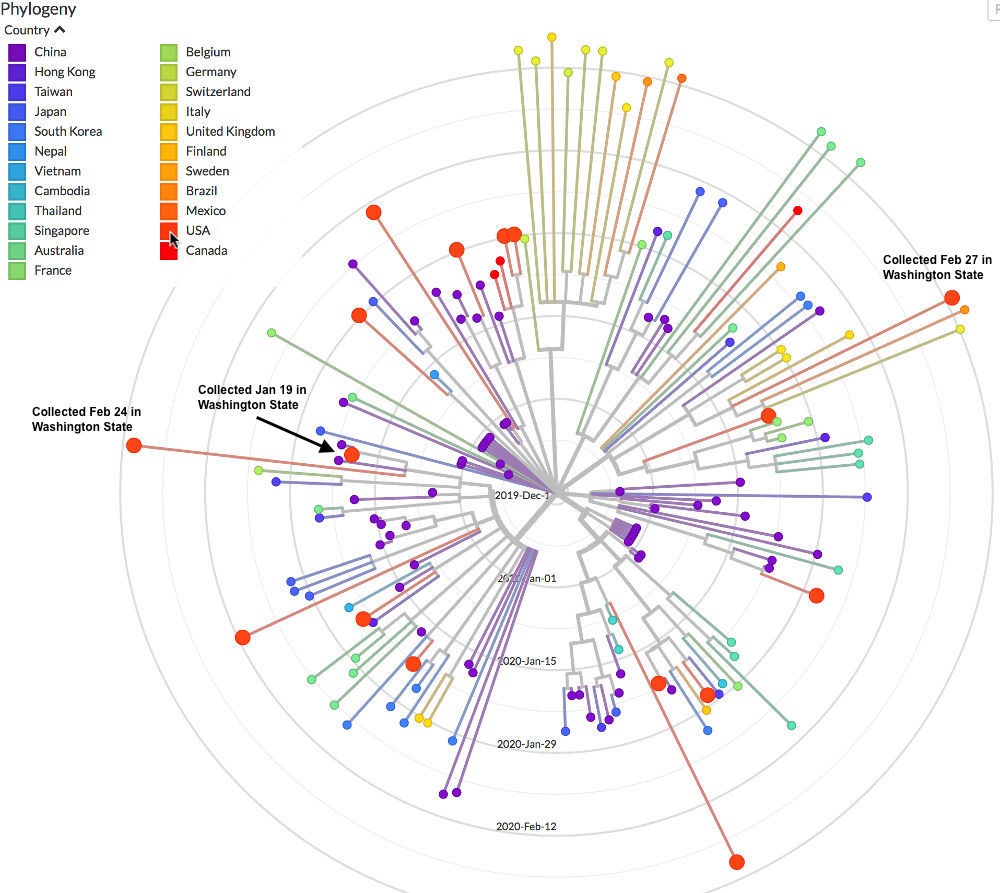
The best one is where genetic sequencers are now sharing the virus genome using Github to make this beautiful map of the evolution of the COVID-19 virus. As I had explained in the original post, Coronavirus is an RNA virus, which is prone to frequent mutations. Most mutations are minor and do not ultimately affect how virulence (deadliness) or transmissiblility. (There is now a report of two minor strains with different virulence, one in Wuhan in particular, but this has not been widely corroborated.) Biologists estimate that it mutates at 2 nucleic acid mutations a month. So we essentially track the virus as it spreads throughout the world and know with pretty good certainly how it hopped from place to place. Here I've hovered over the USA, so the big red dots are the ones in the US. 3 dots were in Washington State, collected on January 19, February 24, and February 27. The one collected on January 19 appears to be closely related to the one collected on February 24. The one collected on February 27 is more closely related to others collected in Europe. Based on the wide genetic differences between the various US cases, there have been multiple introductions of the virus from various places, not just China.
Question: I understand that you can be contagious before you show symptoms, but is the virus itself somehow more transmittable than other viruses? Like, if an infected person coughs and leaves SARS-CoV-2 on a surface, is it more likely to infect someone than if it was just a normal cold virus?
Answer: There are too many types of cold viruses to be able to make that comparison. Five "cold" viruses are actually coronaviruses that are much milder than what we are dealing with. I'd say it's more transmissible than some. A quick search for flu shows this: viruses survived for 1-2 days on hard surfaces. Previous Coronaviruses have been tested, and the average is 5 days on hard surfaces. But it may not be an apples to apples comparison. That's the thing about trying to interpret science studies. You really have to dig into data to find out how much virus was put on the surfaces in the first place and how the virus was collected from the surfaces days later and how the final sample was tested. All of these things can make a world of difference. Plus, just because virus can be detected in a laboratory from a surface doesn't mean it was enough virus to cause illness.
Question: Can an infected person transmit it by breathing & talking in your face or spitting in your food?
Answer: breathing & talking in your face - yes
spitting in your food - yes
breathing and talking 6 feet away - far less likely
touching a surface with grimy hands and then someone else come along to touch it a few hours later and then rubbing their nose - yes and the most likely method of transmission
March 3, 2020 4:30 p.m.
Question: Could you make it more clear if your charts about deaths, cases are for the entire U.S. or are indicative of a smaller geographic area? I think I understand that you've time-shifted the data backward to line up with the first death between your earlier projections and the newer projections, but there's very little discussion of the population size that goes along with the projection data? Thanks very much for your writing on the matter and for sharing your expertise and observations as a doctor and a business owner.
Answer: Excellent questions. My chart about deaths and cases apply to an area where people would likely have regular contact with each other. Originally I had thought about it from an entire US standpoint, but now that Seattle is the first area affected, I've been rethinking about how this growth model really applies better regionally. How big is a region? I'd say a metropolitan area. So the entire Seattle area would include the suburbs where people live and commute into the city, about 3.5 million people.
My chart uses basic math of infection rate and time-shifting to correlate deaths to infected people. It does not take into account the population (doesn't need to), saturation of population, overcrowding of hospitals, continued source of imported cases, social distancing, or viral mutations. What I projected holds true in the early phases of an epidemic - very math based. Things that happen later in an epidemic like social distancing/soft quarantine (slows down spread) or hospital overcrowding (increases mortality) are too hard to predict. That's why I cut off my projections a few months in. Once people start dying, we don't know for sure how other people will react and how the government will react.
Since we aren't able to test everyone (due to not enough test kits and criteria for testing criteria too stringent), we don't know how many people are currently infected -- and infectious. The only way is to guess, working backwards from confirmed deaths. As of this writing, there are confirmed 9 deaths. If my assumptions are close, then there are 5000+ infected people in Seattle. But could there have been more than 9 deaths, some not confirmed for Coronavirus in that area? My gut says yes, and I feel there are probably closer to 10,000 infected people in the Seattle area. That means in a week, the hospitals in the area will have an extra few hundred patients. I'd have to do a lot of research to find out how many hospital beds they have in the metropolitan area, but they might be able to accommodate that number. If they don't start closing schools and discouraging mass gatherings though, the number infected will continue to grow and eventually overwhelm hospitals in 2-3 weeks.
In other news...
Dr. James Robb from UCSD who used to do Coronavirus research sent out an email that has gone "viral," and it appears from reporters trying to source verify to be legitimate. He's apparently been doxxed, poor guy. He makes a few suggestions like taking Zinc lozenges. An article from 2010 looked at in vitro (in a lab, not in a human) zinc on Coronaviruses, showing that zinc did have an impact. From my experience as a doctor, I can't say that it has a noticeable effect. I looked for a well-researched link and found this 2011 meta-analysis that showed zinc effectiveness for colds was inconclusive.
If you don't see any left on the shelves, don't be upset. Even if it "helps," it might only reduce symptoms by a day for 10% of people and certainly won't prevent anyone from dying. The ideas about not touching anything in public with your hands and sanitizing shopping carts and other shared equipment is all pretty common sense. He's pretty pro-mask and pro-gloves. That's easy for a scientist/doctor to say to his colleagues. For most people not used to wearing disposable gloves, the correct usage of these this sort of equipment is more important than having them. The key is still to not touch random surfaces and then your nose, mouth, or eyes (which are connected to your nose where the receptors for the virus are).
The New England Journal of Medicine is a very prestigious journal historically. The latest issue has a few editorials from prominent people, including Bill Gates and Dr. Fauci. For anything your read, consider the source and their agenda.
March 3, 2020 10:00 a.m.
I find it disappointing that the CDC has changed the way they are reporting. As discussed in the original post, the denominator is critically important to understanding what's going on. If you don't test very many cases, you won't detect very many cases. We know that last Friday, there were 472 tests performed in the US. Because that's obviously too low and doctors are going on national TV complaining about not being able to test patients, the CDC has changed their reporting to leave off the number of tests performed. Instead, they are putting out "feel good" numbers like there have only been 15 new cases yesterday. Well, is that 15 new cases because we only tested 15 people from the affected nursing home? Or is it 15 new cases for the entire population of King County/Seattle (2,300,000+ people)? The denominator is what really tells us what's going on. When the CDC leaves that off from their reporting, the numbers they are putting out are nearly useless. This chart is from February 28, 2020. It shows the denominator.
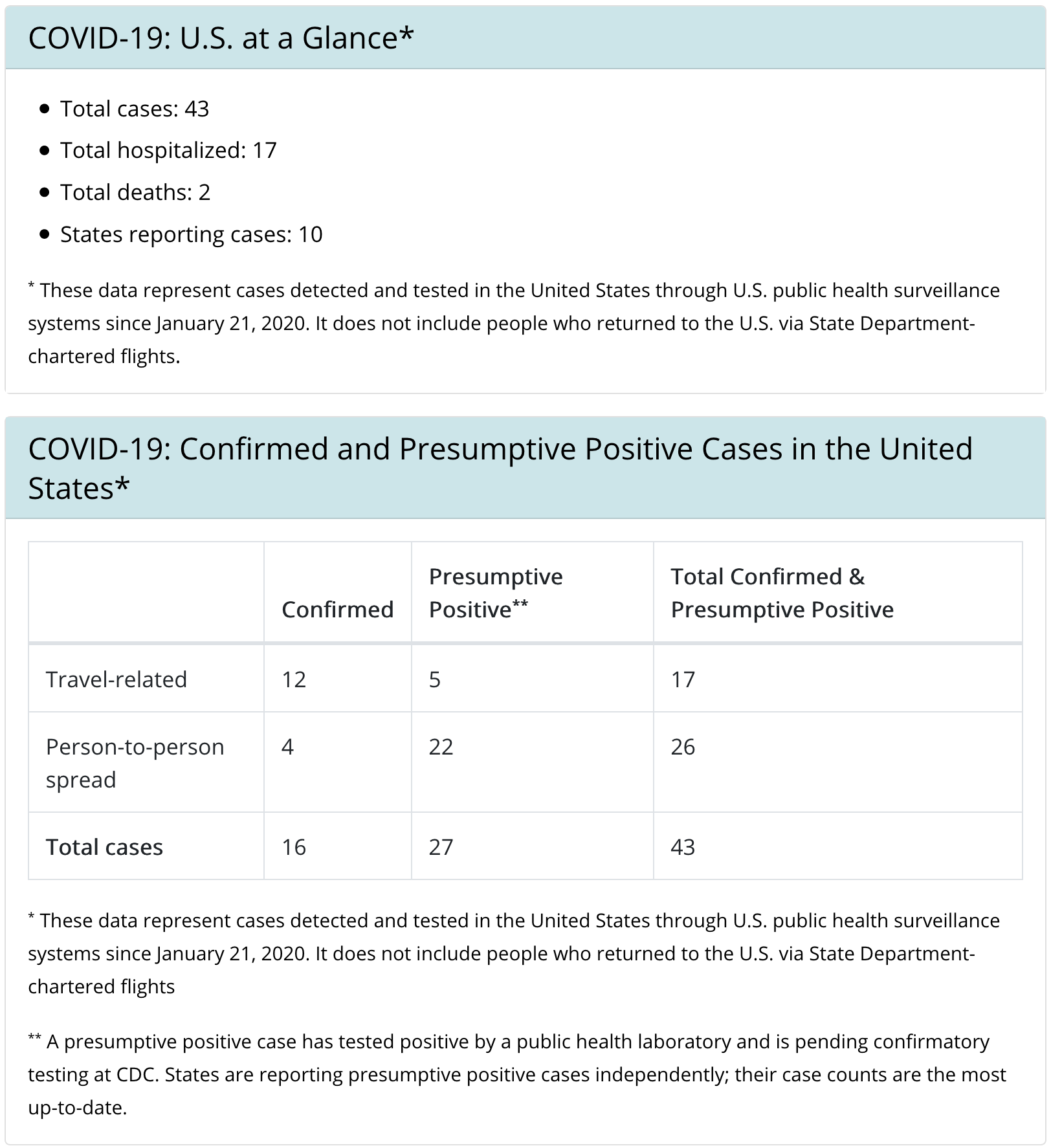
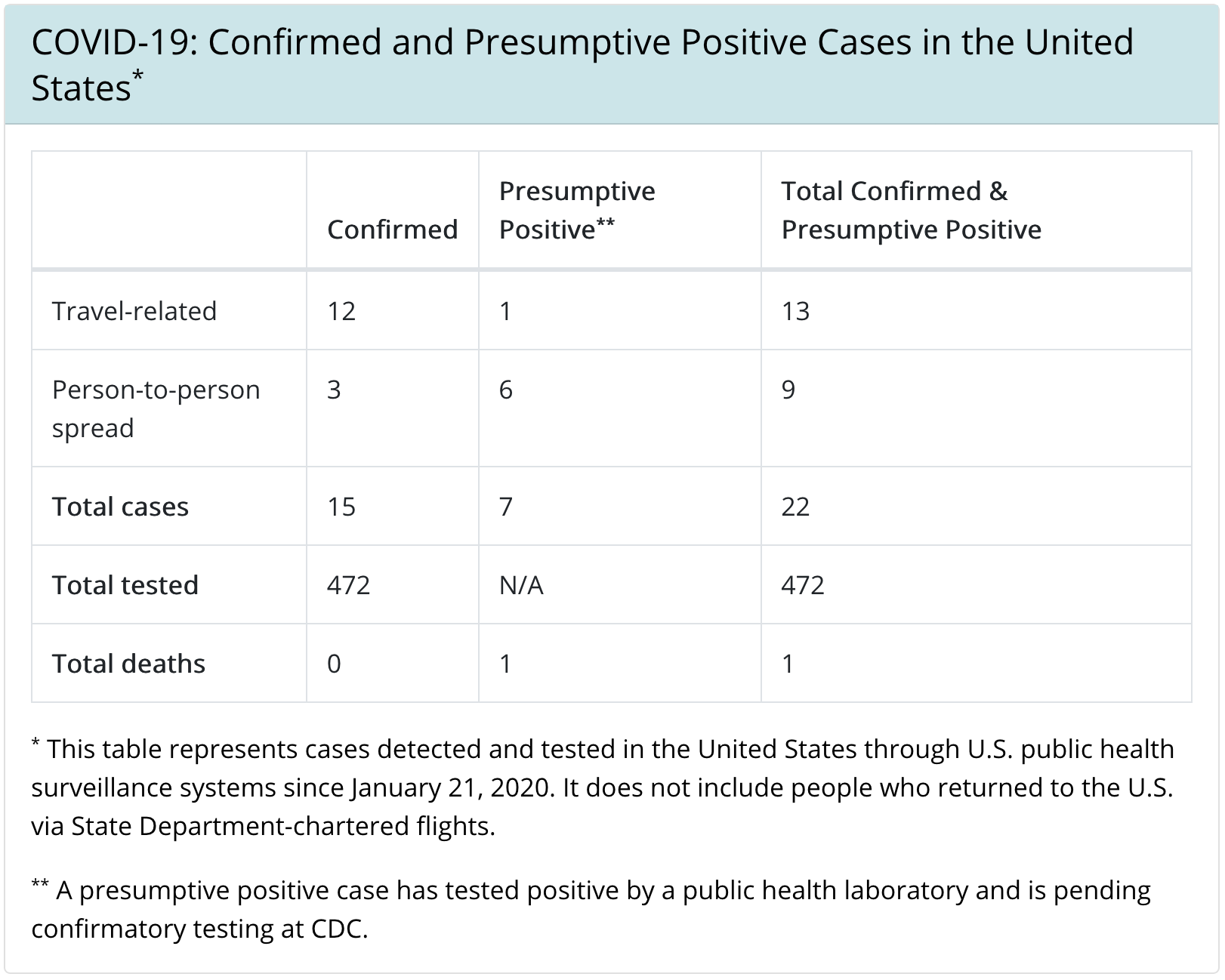 This chart is from March 3, 2020. Reporting has been deliberately changed. Note that at the beginning of yesterday, there were 2 deaths. By the end, there were 6. This chart was a screen capture from today. But the CDC is only updating this chart Monday, Wednesday, and Friday at this time.
This chart is from March 3, 2020. Reporting has been deliberately changed. Note that at the beginning of yesterday, there were 2 deaths. By the end, there were 6. This chart was a screen capture from today. But the CDC is only updating this chart Monday, Wednesday, and Friday at this time.
Also, as of last night, 6 deaths have been confirmed, all in the Seattle area (one case is slightly North of King County). According to my chart, for there to be 6 deaths, there would be 3000+ cases in the area. It hit a nursing home and a hospital particularly hard, where the population is most vulnerable. This is of course expected. It's consistent with the high mortality rate in the elderly. LifeCare Nursing Home has 100+ residents and 180 staff, according to Seattle Times. 50 people related to LifeCare are under investigation. Disease clusters are to be expected, especially for nursing homes. Here is a slightly easier-to-read summary of the King County case load.
| M/F | Age | Disease Cluster | Status |
| M | 50's | Highline Hospital | Critical |
| M | 70's | LifeCare Nursing Home | Died 3/1/20 |
| F | 70's | LifeCare Nursing Home | Died 3/1/20 |
| F | 80's | LifeCare Nursing Home, now at EvergreenHealth Hospital | Critical |
| F | 80's | EvergreenHealth Hospital | Died 3/1/20 |
| F | 90's | EvergreenHealth Hospital | Critical |
| M | 70's | EvergreenHealth Hospital | Critical |
| M | 70's | EvergreenHealth Hospital | Died 2/29/20 |
| M | 60's | Valley Medical Center | Hospitalized |
| M | 60's | Virginia Mason Medical Center | Hospitalized |
| F | 50's | South Korea Travel | Recovering at home |
| F | 70's | LifeCare Nursing Home, now at EvergreenHealth Hospital | Hospitalized |
| F | 40's | LifeCare Nursing Home, now at Overlake Medical Center | Hospitalized |
| M | 50's | EvergreenHealth Hospital | Died 3/1/20 |
There was another man in his 40's from nearby Snohomish County, treated at Evergreen Health who also died on 3/1/20.
It appears that some school systems in the area are closed, but most remain open. While children don't have severe symptoms, they are likely to carry the virus to spread to other people. For the rest of us not in that area, we will observe how this situation plays out over the next 2-4 weeks with hospital crowding and deaths. Then we can adapt that scenario to our own communities. If they don't shut things down at 6 deaths out of 2.3 million people in the suburbs of a major metropolitan area, will the area hospitals be able to handle the number of cases needing oxygen and critical care ventilators? If so, great! We all have a bit more time to prepare.
March 2, 2020 4:00 p.m.
Last night, an acquaintance near NYC was worried that their local Target was completely out of paper products, fever reducers, and hand sanitizers.
Locally, my grocery store in Erie, PA still has cold medicines in stock as of today at noon. The hand sanitizer and isopropyl alcohol sections are running very low. Don't panic! This is to be expected. People are buying what they need to weather the storm. Supply chain is still in place, and these will be replenished but sell out quickly again.
If you are in a major city (my definition is having a subway system), it would make sense to visit your store 1-2 times a week to keep your refrigerator stocked up with your favorite fresh foods (but don't overdo it) and check for supplies when they restock. Social distancing measures (school closures, discouraging mass gatherings, non-essential business closure) may occur in the next few weeks, sooner if you are on the West Coast. If you are in a secondary city (my definition is having a public bus system), evaluate whether you've had confirmed cases locally. If you have a confirmed case, then follow my recommendation for the major cities to stock 1-2 times weekly. If you are in a rural area, keep up with the news and slowly prep for school closure, especially when cases appear closer to home.
This page has my recommended supplies list to weather a soft quarantine event at the very bottom.

March 2, 2020 10:00 a.m.
This CDC page updates how many tests for Coronavirus we've done in the US. On Friday Feb. 28, we had performed 472 tests, finding 22 cases. We will see what today's update reveals. Our factories in Shenzhen are reporting increasing production. One is at 80% of workers, with no major problems getting their supplies. The other is at 30% workers, with no shipping cartons or magnets left. They do still have about 20 days of circuit boards. Both factories anticipate getting back to 80-90% capacity by late March to April 2020. Schools in China may not open until May. That causes problems because younger kids would need at-home childcare, so only one parent can work. Even if the grandparents are part of the household, the kids need to log into the school system using their mom's mobile phone. Neither the kid or the grandparents would have a mobile and know how to log in to the school to report progress. There was one imported case in Shenzhen in recent days, brought in by someone traveling from England. This is the new problem for China - keeping the disease out, while continuing to stamp it out of the hot zones.
March 1, 2020 9:00 a.m.
Question: How does the testing for the virus work? If this virus is similar to a cold virus how do we know if someone has this particular virus? Also how much faith can we give to the CDC in really understanding this?
Answer: There are two types of tests that are being used and developed. One is a blood test just developed by Singapore two days ago, so that's not widely available yet. That one is highly accurate and can detect people who never had symptoms.
The one that is currently being being used around the world uses RT-PCR, which looks for short sequences of genetic code exclusive to this virus. It's essentially a genetic test for the virus, like 23andMe is a genetic test kit for humans. It's quite accurate as well as long as the nose swab, throat swab, and coughing mucus (sputum) samples are collected reliably. (Sometimes I wonder if the nurse swabbing my squirming kid for strep actually got anything on the stick, you know?) No test is 100% however, so right now to confirm a case, two rounds of testing are being done. One at a state or regional lab and then confirmation by the CDC. It takes up to four days to get the final confirmation right now. (It's getting faster as we speak.) The CDC understands it. It's really not all that mysterious. There are tons of armchair scientists like me who understand this stuff too. Anyone with a slightly advanced biology degree in the past 30 years has a basic understanding of the PCR process. Public health officials from the CDC have to be very very careful with what they say. Once they make an announcement about anything, it's now officially coming from the government. They loath denying or confirming anything until all facts are in, so they will always be the last one to make a declarative statement, lest the government be sued by its own people.
Question: Anyone consider preventatively using chloroquine phosphate (an anti malaria drug) that's showing some promise in preventing COVID-19 infections?
Answer: Depends on age, dose, and other health conditions, but widespread recommendation of using this as a prevention may cause more harm than good.
Question: There is a case in my city. Should I keep my 7 year old home?
Answer: I'm on a forum with other scientists discussing this. Everyone says it's the responsible thing to do in the interest of public health. Kids staying home can help protect nursing home folks from dying. There is some discussion on the science side of things, and this is in the WHO report: "Data on individuals aged 18 years old and under suggest that there is a relatively low attack rate in this age group (2.4% of all reported cases). Within Wuhan, among testing of ILI samples, no children were positive in November and December of 2019 and in the first two weeks of January 2020. From available data, and in the absence of results from serologic studies, it is not possible to determine the extent of infection among children, what role children play in transmission, whether children are less susceptible or if they present differently clinically (i.e. generally milder presentations). The Joint Mission learned that infected children have largely been identified through contact tracing in households of adults. Of note, people interviewed by the Joint Mission Team could not recall episodes in which transmission occurred from a child to an adult." I'll try to find out how testing was done in China for kids. As comprehensive as the current CDC guidelines of nose swab, throat swab, and sputum sample? Doubt it. It's probably just a throat swab on a squirmy kid who pulls back and shoves the stick out of their mouth with their tongue while kicking the nurse. PCR on that sample for a relatively asymptomatic (lower viral load with little mucus production) kid may not be very accurate.
Question: Do you think the warm weather will slow the spread?
Answer: Yes, slightly. It will kill viruses from surfaces faster. That will cut down on how quickly the virus spreads, just like closing schools will cut down spread. It may help with the projections a bit.
Question: Is the package I got from China via EMS safe to open?
Answer: It depends on when it was shipped and where it was shipped from. A USPS worker just tested positive in the US. We don't have firm results for this particular Coronavirus yet. In testing of previous Coronaviruses, they have been known to stay on a variety of surfaces for days. Under ideal conditions, it can be detected even a month later. Detection via lab tests doesn't mean it's enough to cause an infection. This research paper has a table that should be pretty straightforward for anyone to understand.
I'd say a 5 day period between when it was shipped to when you open it is generally safe. If you are seriously concerned about decontamination procedures - I don't think most healthy people would need to be, carefully open the package and remove item with gloves. Then leave it in a sunny, warm location to get aired out for a few days. If you only have fabric gloves, that's okay. Just wash them. Detergent and warm water in a washing machine cycle will take care of the virus. If the item can be wiped down, you can use clorox wipes, a dilute bleach solution, alcohol wipes (paper towel with 70% isopropyl alcohol for example), or hydrogen peroxide wipes. I think it's way overkill for most people, but if you care for someone medically fragile, these are some easy tips. The CDC site has details as well.
February 29, 2020 6:00 p.m.
News broke today that a man in King County, Washington State has died from COVID-19. He did not travel to any high-risk countries, so this was a death caused by community spread. There are no details yet for when he began exhibiting symptoms. He was in his 50's and had other health conditions that may have caused him to have worse illness than healthy people in their 50's.

My previous predictions were based on the woman with severe illness near Sacramento. That chart did not predict a first death until mid-late March. Now that there is a first death on Feb. 29, I went through to re-date the numbers. The math in the predictions doesn't change very much.
Based on further information, I've modified my assumptions slightly to create a new chart.
- R0 remains 2.0 for the US, since we use less public transport, live farther apart, and contact fewer people on a daily basis than in China. R0 in China is estimated at 2.3, though some epidemiologists are using a value of 6, which would really be a bad scenario.
- Each generation is 8 days. This is based on SARS and MERS data, since they are other coronaviruses for which we have pretty good historical data. Some epidemiologists are using 3-7 days for COVID-19, but I'll continue to use 8 days.
- Mortality in China was 2%, and I used 1% previously thinking that Americans are a slightly healthier lot and the the medical care here is better. I'm going to dial it in at 1.2% now, just to play with the numbers a bit.
- I had used 28 days from infection to death previously. I'm changing it to this now: 5 days from infection to symptoms starting (5.5 day average for China, but we're talking about older, sicker people, so going with slightly less) + 4 days to hospitalization (based on my experience as a doctor for older people) + 11 days in the hospital before death (also just doctor experience and only while we have enough hospital beds for oxygen and ICU beds with ventilators) = 20 days from infection to death.
- This again assumes no social distancing/quarantine conditions.
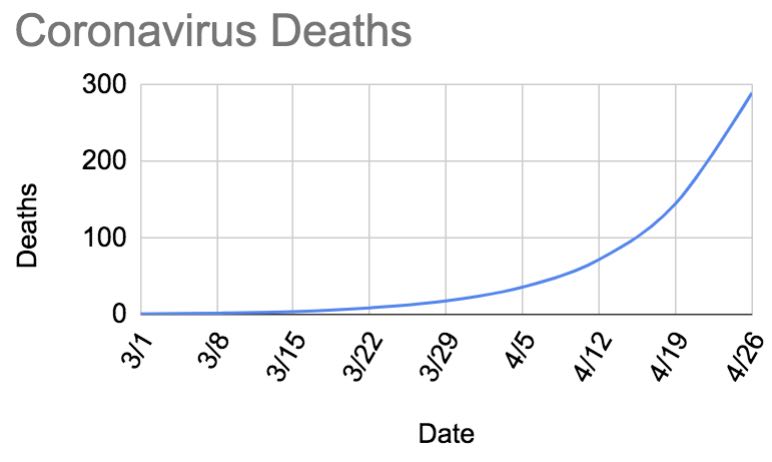
I appreciate everyone's comments and encouragement for my previous post. I'll provide updates here as we receive more information. The numbers are quickly changing since we finally started testing. We've only tested a few hundred suspected cases. I expect that over the next few days, we will see more severe cases and deaths. At that point, I'll adjust the dates to match the new numbers. We may be closer to a few thousand community cases than just 500 cases because we haven't been testing adequately. This is a very conservative estimate of case load.
As for when to expect cases in major cities, I think it's already in all major cities. My previous timeline was off by about 2-3 weeks. I thought we may have been about a month away from shutting down travel, but I think that the announcement would be coming in 1-2 weeks. I feel like there is a 50% chance that my kid who is home for Spring Break this first week in March will likely not return to school after break.